Table of Contents >> Show >> Hide
- What the Test Measures (and Why Cosyntropin Gets an Invite)
- Why a Clinician Might Order an ACTH Stimulation Test
- Types of ACTH (Cosyntropin) Stimulation Tests
- How to Prepare (Without Accidentally “Studying for the Test”)
- What Happens During the Test
- How Results Are Interpreted (and Why the “Normal” Number Isn’t One Number)
- Important Limitations and “Gotchas”
- What Happens After the Test
- Frequently Asked Questions
- Real-World Experiences: What It’s Like to Actually Do an ACTH Stimulation Test (About )
- Conclusion
If your body had a “stress thermostat,” cortisol would be one of its main dials. It helps regulate blood pressure,
blood sugar, inflammation, and how you respond when life throws a surprise plot twistlike a stomach bug, a
surgery, or the kind of meeting that could’ve been an email.
The ACTH (cosyntropin) stimulation test is a common way clinicians check whether your adrenal
glands can “turn up the cortisol” when prompted. It’s widely used to evaluate
adrenal insufficiency (when the body can’t make enough cortisol), and it can also help clarify
where the problem might beat the adrenal glands themselves, or higher up in the hormonal chain.
This article explains what the test is, why it’s ordered, how it’s done, what results can mean, and why two people
can get the “same” test but not the same reference range. We’ll keep it medically groundedwhile still allowing
the occasional moment of humor, because healthcare is serious and also sometimes absurd.
What the Test Measures (and Why Cosyntropin Gets an Invite)
Your cortisol system is part of the HPA axisthe hypothalamus, pituitary, and adrenal glands.
In simple terms:
- Hypothalamus and pituitary send signals.
- The pituitary releases ACTH (adrenocorticotropic hormone).
- ACTH tells the adrenal glands (on top of your kidneys) to make cortisol.
Cosyntropin is a synthetic form of ACTH used as the “signal” in the test. Think of it like
pressing a doorbell:
- If the adrenal glands are working and able to respond, cortisol should rise after cosyntropin.
- If cortisol barely budges, it suggests a problem with adrenal function or adrenal reserve.
Because cortisol is essential for life, diagnosing true adrenal insufficiency matters. Untreated, severe cortisol
deficiency can lead to dangerously low blood pressure and an emergency known as adrenal crisis.
Why a Clinician Might Order an ACTH Stimulation Test
The test is usually ordered when symptoms, medical history, or earlier labs raise concern that cortisol production
might be too lowespecially in the morning when cortisol is typically higher.
1) Suspected adrenal insufficiency
Adrenal insufficiency can be:
-
Primary adrenal insufficiency (problem at the adrenal glands themselves; Addison’s disease is
a well-known cause). - Secondary adrenal insufficiency (problem at the pituitary, which makes ACTH).
- Tertiary adrenal insufficiency (problem at the hypothalamus, which signals the pituitary).
Symptoms can be vaguefatigue, weakness, dizziness, nausea, weight loss, low appetite, or low blood pressure.
Sometimes the “symptoms” are actually the labs: low sodium, high potassium (more suggestive in primary adrenal
insufficiency), or low morning cortisol.
2) Possible adrenal suppression from steroid medications
Long-term glucocorticoid use (like prednisone, hydrocortisone, or steroid injections in some settings) can suppress
the HPA axis. When the body senses steroids coming from outside, it may reduce its own ACTH and cortisol production.
The ACTH stimulation test can help assess whether the adrenal glands are ready to resume normal function.
3) Evaluation for certain adrenal enzyme disorders (including CAH in specific contexts)
In some cases, ACTH stimulation testing supports evaluation of adrenal steroid pathwayssuch as suspected
congenital adrenal hyperplasia (CAH) variantsoften alongside additional hormone measurements ordered by specialists.
Types of ACTH (Cosyntropin) Stimulation Tests
Most people mean one of two versions when they say “ACTH stimulation test.” Your clinician and lab protocol decide
which one is appropriate.
Standard-dose (high-dose) test: the classic
The most common version uses 250 micrograms (mcg) of cosyntropin given by IV or IM injection.
Blood is drawn for cortisol before the dose, then again after the doseoften at 30 minutes and
60 minutes. Some protocols include additional time points.
Low-dose test: the “small but mighty” option
Some endocrine practices use a 1 mcg low-dose protocol in specific situations, often to evaluate
milder or earlier secondary adrenal insufficiency. It can be more finicky because it requires careful dilution and
precise administration. Translation: it’s a great test when done well, and a confusing test when done sloppily.
If you’re unsure which one you’re getting, don’t worryyour ordering clinician almost always knows which protocol
they intended, and the lab order typically spells it out.
How to Prepare (Without Accidentally “Studying for the Test”)
Preparation varies by facility and your medical context, so follow the instructions you’re given. But these are
common themes clinicians consider:
Timing matters
Many facilities schedule the test in the morning, when baseline cortisol is easier to interpret
relative to typical daily rhythms.
Food and fasting
Some centers ask you to fast for several hours beforehand; others allow a light meal. If your instructions include
fasting, don’t “negotiate” it with a muffin. (Okay, you can negotiatejust do it with the clinic staff.)
Medication review: this is a big one
Certain medications can affect cortisol measurements or the HPA axis. The most important category is
glucocorticoids (steroids), including pills, injections, and sometimes high-dose topical or
inhaled steroids.
Do not stop steroids on your own. If your clinician wants you to hold a dose before the test,
they’ll tell you exactly how and when. Holding the wrong steroid at the wrong time can be unsafeespecially if you
truly have adrenal insufficiency.
Also tell your clinician if you take estrogen-containing medications (including some birth
control and hormone therapy). Estrogen can affect cortisol-binding proteins and may change total cortisol readings.
What to bring
- A list of medications and supplements (or photos of the bottles).
- A snack for afterward (if allowed), because waiting around hungry is a personality test nobody asked for.
- A short-sleeve shirt or something with easy arm access for blood draws.
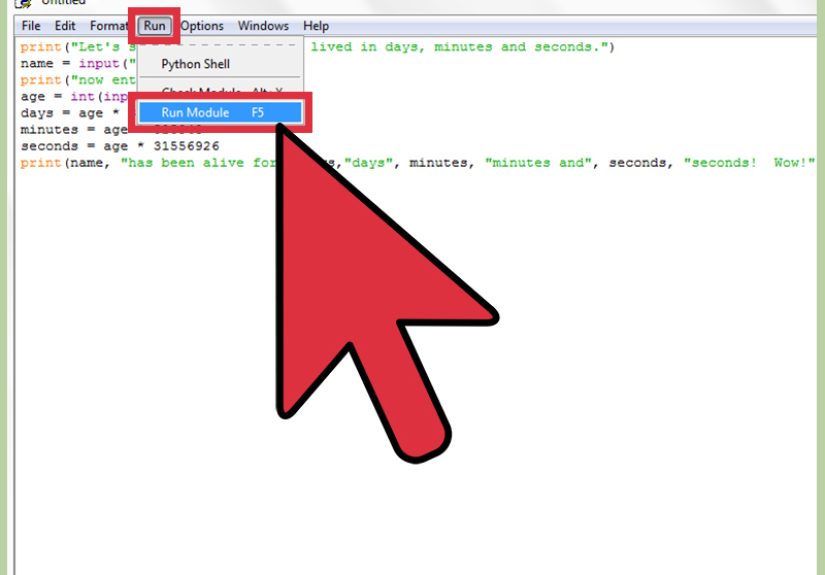
What Happens During the Test
Most ACTH stimulation tests take about 1 to 2 hours start to finish, depending on the protocol.
Here’s the typical play-by-play:
Step 1: Baseline blood draw
A nurse or phlebotomist draws your baseline cortisol level (and sometimes ACTH or other hormones, depending on what
your clinician ordered).
Step 2: Cosyntropin is given
Cosyntropin is administered via IV (often as a quick push) or IM injection,
depending on the center.
Step 3: Timed blood draws
Blood is drawn again at specific time pointscommonly 30 minutes and 60 minutes
after cosyntropin. Some protocols add a 15-minute draw or other intervals.
Step 4: You go live your life
Once the final blood draw is done, you’re usually free to leave. Some clinics observe you briefly after the
injection, especially if you have a history of medication reactions.
Side effects and safety
Most people tolerate cosyntropin well. Possible short-lived side effects can include flushing, mild nausea, or a
“huh, that was weird” feeling for a few minutes. Serious allergic reactions are uncommon, but clinics are prepared
to respond if they occur.
How Results Are Interpreted (and Why the “Normal” Number Isn’t One Number)
The basic idea is simple: cortisol should rise after cosyntropin. The details are where medicine
does its favorite thingcomplicates the group project.
Common interpretation approach
Historically, many references taught that a peak cortisol of about 18 mcg/dL (500 nmol/L) at 30 or
60 minutes suggests an adequate response. However, newer, more specific cortisol assays (including certain
immunoassays and LC-MS/MS methods) can yield lower numeric values, and research supports
assay-specific cutoffs that may be closer to the mid-teens in some labs.
That’s why your report’s reference range matters. The most practical rule for patients is:
interpret your result using your lab’s reference interval and your clinician’s context, not a
single universal cutoff from the internet (even if the internet is very confident and uses ALL CAPS).
Primary vs. secondary adrenal insufficiency
The ACTH stimulation test evaluates adrenal response, but it doesn’t always pinpoint the cause by itself. Clinicians
often pair it with baseline ACTH and other labs:
-
Primary adrenal insufficiency: adrenal glands are the main problem. Baseline ACTH may be high
because the pituitary is “shouting” but the adrenals aren’t responding. -
Secondary/tertiary adrenal insufficiency: ACTH signaling may be low or inadequate, and the
adrenal glands can become under-stimulated over time.
Borderline results aren’t rare
Sometimes results are clearly normal or clearly abnormal. Other times they fall into a gray zoneespecially if
you’re recovering from steroid exposure, have recent pituitary disease, are acutely ill, or your lab uses a newer
assay.
In borderline cases, clinicians may:
- repeat testing under standardized conditions,
- use additional labs (ACTH, renin/aldosterone, electrolytes),
- consider alternative dynamic tests in specialty care, or
- treat presumptively if clinical risk is high.
Two quick examples (numbers are illustrative)
Example A: Baseline cortisol is low at 8 a.m., but after cosyntropin it rises robustly into the
lab’s “pass” range at 30–60 minutes. That pattern suggests the adrenal glands can respond appropriately, and your
clinician may look for other explanations for symptomswhile still considering pituitary history if relevant.
Example B: Baseline cortisol is low and barely increases after cosyntropin, staying below the
lab’s expected stimulated range. Combined with symptoms and supportive labs, this strengthens the case for adrenal
insufficiency and usually triggers a next-step evaluation plan.
Important Limitations and “Gotchas”
No test is perfect. The ACTH stimulation test is extremely usefulbut it has known limitations.
Early secondary adrenal insufficiency can be tricky
If pituitary ACTH has only recently dropped (for example, shortly after certain pituitary events or surgeries),
adrenal glands may still respond normally for a period of time. In that situation, a normal cosyntropin response
doesn’t always rule out evolving secondary adrenal insufficiency. Clinicians interpret results with timing and
clinical context in mind.
Recent steroid use can confuse the picture
Steroid medications can suppress the HPA axis and can also interfere with cortisol measurement depending on the
specific medication and assay. This is why your medication history is not “extra info”it’s the plot.
Acute illness and physiologic stress change cortisol dynamics
Severe illness can raise cortisol, alter binding proteins, and complicate interpretation. In emergencies, clinicians
prioritize treatment first if adrenal crisis is suspectedtesting is often secondary to stabilization.
What Happens After the Test
Your clinician will interpret the results in context and decide on next steps. Depending on the situation, this may
include:
- no further adrenal testing if results are clearly reassuring,
- additional labs to determine primary vs. secondary causes,
- endocrinology referral for comprehensive evaluation,
- education about “sick day” steroid rules if adrenal insufficiency is diagnosed,
- and in some cases, starting or adjusting glucocorticoid replacement therapy.
If you’re diagnosed with adrenal insufficiency, it’s common to discuss an emergency plan (including when to seek
urgent care for vomiting, severe weakness, or fainting) and the potential need for medical alert identification.
Frequently Asked Questions
Is the test painful?
Most discomfort comes from the needle sticks. The cosyntropin injection itself is usually brief. If you’re prone to
tricky veins, hydration (when allowed) and warm sleeves can help.
How soon will I get results?
Some labs return cortisol results the same day; others take longer. Ask your clinic what’s typical for their lab.
Why not just do one morning cortisol test?
A single morning cortisol can be helpful, but it’s not always definitiveespecially in the borderline range. The
ACTH stimulation test is a dynamic assessment of adrenal reserve, which can provide clearer information when the
baseline picture is uncertain.
Can I drive afterward?
Most people can. If you tend to feel faint with blood draws, consider having someone come with you or plan a few
minutes to sit and recover before heading out.
Real-World Experiences: What It’s Like to Actually Do an ACTH Stimulation Test (About )
Let’s be honest: “dynamic endocrine testing” sounds like a NASA checklist, and the phrase “we’ll draw your blood
several times” is not exactly a spa slogan. But most people walk away saying some version of:
“That was way less dramatic than I expected.”
A common experience is the waiting-room mental montage. You arrive early because the appointment
is in the morning, you’ve googled “cortisol” at least once, and now you’re wondering whether you should be feeling
stressed because the test is about stress hormones. (You’re not “ruining the test” by being nervous. Humans are
allowed to be humans.)
The first surprise for many people is how ordinary the process feels. You check in, someone places
an IV or draws blood, and then you sit. The clinic may ask you to stay seated and relaxed between draws. This can
feel mildly ironic in a world where sitting quietly without checking your phone is basically a competitive sport.
Bring something easy: a podcast, a short book, a playlist, or the kind of brainless game that doesn’t raise your
blood pressure like online shopping.
People often describe the cosyntropin injection as a “non-event.” Some feel nothing. Some notice a brief warm flush
or mild nausea that passes quickly. A few say they felt slightly “amped” or strange for a moment, and then it was
gone. The more annoying part is usually the clock watching: you become intensely aware of what 30
minutes means, like you’re waiting for bread to toast but the toaster is your endocrine system.
If your veins are shy (or just stubborn), the experience may revolve around hydration and vein strategy. People who
have had multiple blood draws in the past often show up with practical wisdom: wear sleeves that roll up easily,
drink water if permitted, and don’t be afraid to say, “My left arm is usually better,” because you are the leading
expert on your left arm.
The emotional part often hits after. Some people feel relief just for having a planbecause vague
symptoms can be exhausting, and testing can make things feel more concrete. Others feel anxious waiting for results,
especially if they’ve had scary episodes of dizziness, fainting, or unexplained fatigue. A helpful mindset is to see
the test as a flashlight, not a verdict: it shines light on one part of the story, and then your clinician uses that
light to decide the next step.
Parents of children doing the test (or adults supporting a loved one) often mention that the hardest part is
logistics: scheduling, fasting instructions, keeping kids calm, and making time for follow-up. The most useful tip
is simple: ask the clinic ahead of time how long you’ll be there and what your “after plan” should be (snack, meds,
school/work timing). It doesn’t make the needles disappear, but it makes the day smoother.
In the end, many people leave thinking: “I spent more time waiting than anything else.” Which is oddly
comfortingbecause if your adrenal glands are having a hard time, you’ve already had enough drama.
Conclusion
The ACTH (cosyntropin) stimulation test is a practical, widely used tool for evaluating how well
your adrenal glands can produce cortisol when prompted. It’s most commonly used to assess suspected adrenal
insufficiency and can play a role in evaluating adrenal suppression or certain adrenal enzyme conditions in
specialist care.
The test itself is usually straightforwardbaseline blood draw, cosyntropin, timed blood drawsand the most
important part is interpretation: results depend on your clinical context, your lab’s assay and reference ranges,
and any medications or recent health events that can affect cortisol dynamics.
If you’re undergoing testing, the best move is to partner closely with your clinician, share your full medication
history, and ask what the next step will be for both normal and abnormal results. That way, no matter what the
numbers say, you won’t be left staring at a lab report like it’s a cryptic fortune cookie.