Table of Contents >> Show >> Hide
- Statins in Plain English: What They Do (and What They Don’t)
- Who’s “Eligible” for Statins? The Short Version of the Guidelines
- The 35% Statin Gap: What the Data Actually Shows
- Why Aren’t Eligible Adults Taking Statins? It’s Not One ReasonIt’s a Stack
- 1) “I feel fine” is a powerful (and understandable) argument
- 2) Risk calculators are useful, but they’re not “fast food”
- 3) Statin misinformation spreads faster than LDL
- 4) Side effects are realbut fear of side effects is bigger than the average risk
- 5) “Statin intolerance” is often more flexible than the internet implies
- 6) Access, cost, and continuity of care still shape what happens
- 7) Trust and communication gaps are cardiovascular risk factors in disguise
- Side Effects, Nocebo, and Reality: A Calm Look at the Hot Topic
- What Closing the Statin Gap Could Look Like (Without Shaming Anyone)
- Bottom Line
- Experiences From the Real World: Why the 35% Number Feels So Familiar (500+ Words)
Imagine there’s a low-cost, widely studied tool that helps cut your odds of a heart attack or strokeyet most people who qualify never pick it up.
That’s the uncomfortable reality behind a stubborn statistic: statin use for prevention has plateaued, and only about 35% of eligible U.S.
adults report taking them. This isn’t a “people don’t care about their health” story. It’s a “healthcare is complicated, life is busy, and biology
doesn’t send calendar invites” story.
Cardiovascular disease (CVD) is still the heavyweight champion of American health problemsbig, common, and costly. Statins aren’t magic (no pill is),
but they are one of the most proven ways to reduce atherosclerotic cardiovascular disease (ASCVD) risk in the right patients. So why is the uptake so low?
Let’s unpack what “eligible” actually means, what the data says, and what can realistically move that 35% number in the right directionwithout turning
this into a lecture or a guilt trip.
Statins in Plain English: What They Do (and What They Don’t)
Statins are cholesterol-lowering medications that reduce low-density lipoprotein (LDL), often nicknamed “bad cholesterol.”
LDL isn’t “bad” because it’s evilit’s “bad” because too much of it can contribute to plaque buildup inside arteries, which raises the risk of heart
attack and stroke. Statins work by slowing the liver’s cholesterol production and helping the body clear LDL from the bloodstream.
Two points get lost in the internet shouting:
- Statins are prevention tools. You can feel totally fine and still be accumulating risk quietly.
- Statins don’t replace lifestyle. They’re a “both/and,” not an “either/or.” Better food, movement, sleep, and blood pressure control still matter.
In the right groups, statins reduce cardiovascular events enough that most major U.S. guidelines treat them as first-line therapy when risk crosses
certain thresholds. That’s not “pill-pushing.” That’s a risk math decisionlike wearing a seatbelt because physics doesn’t care how confident you feel.
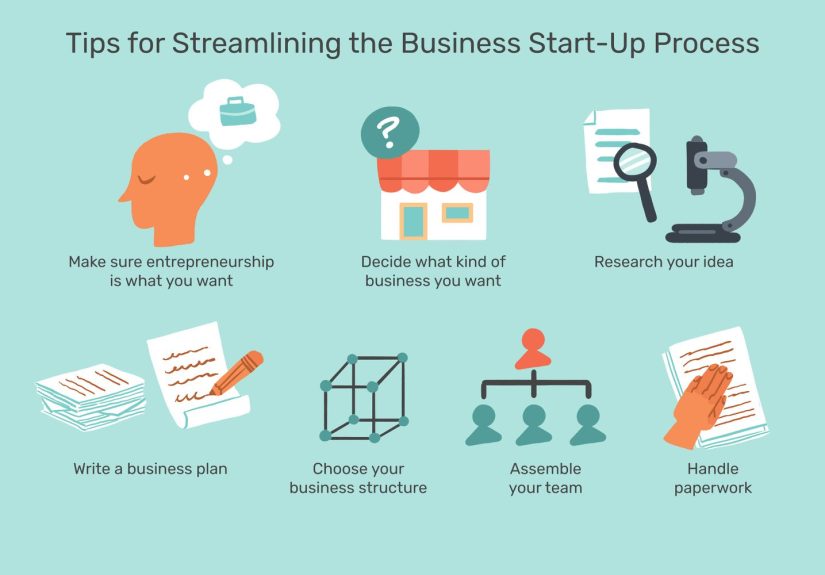
Who’s “Eligible” for Statins? The Short Version of the Guidelines
Eligibility isn’t just “my cholesterol is high.” Modern guidelines focus on overall ASCVD risk. In the U.S., statin recommendations
generally center on a few big categories:
1) Secondary prevention: people who already have ASCVD
If someone has had a heart attack, stroke, or has established atherosclerotic disease, statins are usually recommended unless there’s a clear reason not to.
This is “protect against the next event” territory.
2) Very high LDL (often LDL-C ≥ 190 mg/dL)
Extremely high LDL levels can reflect genetic risk (like familial hypercholesterolemia) and often warrant statins because lifetime exposure to high LDL
can be dangerouseven if you’re currently young and feel invincible.
3) Diabetes (commonly ages 40–75, depending on guideline specifics)
Diabetes increases ASCVD risk enough that many adults with diabetes fall into “statin makes sense” territory, even when LDL isn’t sky-high.
4) Primary prevention based on calculated 10-year risk
This is where the famous risk calculator comes in. Clinicians often use tools like the ASCVD Risk Estimator to estimate 10-year risk based on age,
cholesterol values, blood pressure, diabetes status, smoking, and other factors. Guidelines then recommend or suggest statins when risk is high enough,
with shared decision-making in the borderline ranges.
The important vibe here: eligibility is not about “being a good person who eats kale.” It’s about whether your risk profile predicts enough benefit
that medication is worth it.
The 35% Statin Gap: What the Data Actually Shows
Multiple analyses using nationally representative U.S. data (not “my cousin’s neighborhood Facebook group”) point to the same headline:
statin use rose over time but then stalled. Research using NHANES data from 1999–2018 found that statin use among guideline-eligible adults increased
into the early-to-mid 2010s but plateaued between 2013 and 2018, hovering around that “only about 35%” mark.
Even more eye-opening: the people with the strongest indications aren’t consistently getting treated. In guideline-based analyses, fewer than half of adults
who are recommended statins report taking them. In some high-risk subgroupslike those with very high LDLtreatment rates can be shockingly low.
That’s like installing smoke detectors in only one room because the rest of the house “seems fine.”
Why Aren’t Eligible Adults Taking Statins? It’s Not One ReasonIt’s a Stack
1) “I feel fine” is a powerful (and understandable) argument
High cholesterol and elevated ASCVD risk rarely come with symptoms. People are busy managing what they can feel:
stress, bills, work, kids, sleep, back pain, life. A future heart attack isn’t louduntil it is.
Prevention requires believing a spreadsheet about your future self. Humans are… not always spreadsheet-friendly.
2) Risk calculators are useful, but they’re not “fast food”
Some guideline pathways require multiple inputs, lab results, blood pressure readings, and a patient-clinician discussion. That’s hard in a 12-minute visit
where the patient also wants to talk about knee pain, refills, and why their smartwatch keeps accusing them of being “stressed.”
3) Statin misinformation spreads faster than LDL
Social media is great for recipes and dog videos. It is less great when it turns rare side effects into guaranteed doom.
The result? People show up to appointments already convinced they’ll have muscle pain, memory issues, or “liver failure,” and the conversation starts at
DEFCON 1 instead of “let’s look at your risk and options.”
4) Side effects are realbut fear of side effects is bigger than the average risk
Statins can cause side effects, and some people truly cannot tolerate them. But large randomized trial evidence suggests muscle symptoms attributable to statins
are less common than many assume, and expectation (“nocebo effect”) can play a major role. This doesn’t mean symptoms are “fake.”
It means the brain and body are deeply connected, and the context of taking a medication changes what we notice and how we interpret it.
5) “Statin intolerance” is often more flexible than the internet implies
Modern expert definitions recognize a spectrum: partial intolerance (can tolerate some dose/type) versus complete intolerance (rare).
That matters because many people can do well with adjustmentsswitching statins, changing dose intensity, or using alternative dosing schedulesunder medical guidance.
6) Access, cost, and continuity of care still shape what happens
Statins are generally inexpensive as generics, but access barriers aren’t only about the price of a pill. They’re also about:
getting labs, having consistent primary care, refill logistics, transportation, language barriers, insurance churn, and time off work.
If your healthcare experience is fragmented, preventive care is the first thing to slip.
7) Trust and communication gaps are cardiovascular risk factors in disguise
Some patients feel brushed off. Some clinicians feel constrained. Add a history of pharmaceutical mistrust, rushed conversations, or confusing guideline language,
and it becomes easy to postpone treatment “until next time.” Except next time doesn’t always show up.
Side Effects, Nocebo, and Reality: A Calm Look at the Hot Topic
Here’s the most useful framing: statins are usually well-tolerated, but not universally. Commonly discussed issues include muscle aches,
mild digestive effects, and changes in lab values. Serious liver injury is rare, and routine periodic liver-enzyme monitoring is no longer universally recommended
the way it used to be (testing is typically done before starting and then as clinically indicated).
What about muscle pain? Large trial analyses suggest that the excess risk attributable to statins is small for most people, especially after the first months,
and randomized “statin vs placebo vs no-pill” style studies show symptom patterns consistent with a substantial nocebo contribution.
Translation: if you try a statin and feel muscle symptoms, it deserves a real medical conversationnot an automatic lifetime ban.
Many patients can find a regimen that works.
Practical clinician-style strategies (general information, not personal medical advice) often include:
- Rule out look-alikes (thyroid issues, vitamin D deficiency, intense new exercise, drug interactions).
- Switch the statin (different type, different metabolism, different tolerability profile).
- Adjust the dose (lower dose, gradual titration, or alternative schedules when appropriate).
- Use add-on or alternative lipid-lowering meds when statins truly aren’t tolerated or aren’t enough (based on clinician judgment and indication).
What Closing the Statin Gap Could Look Like (Without Shaming Anyone)
Make risk visible
People can’t act on numbers they don’t know. More consistent cholesterol screening, clearer explanations of LDL and ASCVD risk, and better “here’s what this means for you”
communication can turn statins from “mystery pill” into “specific tool for a specific goal.”
Use team-based care
Pharmacists, nurses, and health coaches can help with education, adherence, side-effect troubleshooting, and follow-upespecially when primary care visits are short.
Prevention works better when it’s supported between visits, not only during them.
Make shared decision-making real (not just a phrase)
Guidelines often encourage clinician-patient discussions because the decision isn’t only clinicalit’s personal. Some people prioritize minimizing meds.
Others prioritize minimizing event risk. The win is aligning treatment with the patient’s values while staying honest about the risk math.
Fight misinformation with specifics, not scolding
“Statins are safe” is too vague to compete with a scary TikTok. Better messages sound like:
“Serious liver injury is rare,” “muscle symptoms caused by statins are uncommon,” and “if symptoms happen, we have options.”
Specifics reduce fear.
Pair medication with lifestyle that actually fits real life
Lifestyle changes don’t need to be extreme to matter. Small, consistent stepsless ultra-processed food, more fiber, regular walking, better sleep,
blood pressure control, quitting smokingstack benefits with statins rather than competing with them.
Bottom Line
Only about 35% of eligible adults taking statins isn’t a failure of one person’s willpower. It’s a system-level story with human-level details:
silent risk, confusing eligibility, rushed visits, misinformation, side-effect anxiety, and uneven access to care.
The opportunity is huge. Better risk assessment, better conversations, better follow-up support, and clearer expectations about side effects could move
prevention from “technically recommended” to “actually happening.” In cardiovascular disease, the quiet choicestaking a daily medication when appropriate,
getting labs checked, showing up for follow-upsoften matter more than dramatic resolutions.
Experiences From the Real World: Why the 35% Number Feels So Familiar (500+ Words)
Statistics are clean. People are not. When you zoom in on everyday experiences, the statin gap starts to make emotional senseeven when it doesn’t make
medical sense.
Experience #1: “My labs were fine… until they weren’t.”
A common storyline goes like this: someone gets a cholesterol test, hears “a little high,” and files it away under “future me problem.”
Years pass. Blood pressure creeps up. Work gets stressful. Sleep gets worse. Maybe weight changes. Maybe blood sugar edges into prediabetes.
None of it feels like an emergency, so prevention feels optional. When a clinician later says, “Your 10-year ASCVD risk is high enough that a statin is recommended,”
it can sound suddenlike the medical system skipped chapters. But the risk didn’t appear overnight; it accumulated quietly. In this experience, the barrier isn’t defiance.
It’s that preventive medicine asks people to act on a gradual trend they couldn’t feel day to day.
Experience #2: The muscle-pain rumor shows up before the prescription does
Many people meet statins first through stories: a friend’s “statin ruined my legs,” a relative’s “I heard it melts your liver,” a headline that turns a rare adverse event
into a certainty. So when a prescription is offered, it’s not arriving in a neutral brain. It’s arriving in a brain that’s already braced for impact.
Then a totally ordinary acheafter yard work, a new workout, or simply aginggets reinterpreted as “the statin.”
The experience becomes self-reinforcing: fear increases attention, attention increases perceived intensity, perceived intensity increases distrust.
That’s why calm, specific counseling and a plan (“If symptoms happen, callwe can adjust”) can be more powerful than reassurance alone.
Experience #3: “I don’t want another daily pill.”
Daily medications carry psychological weight. For some people, a statin feels like a label: “I’m officially unhealthy now.”
For others, it’s a reminder of aging or family history. And for many, it’s just practical fatiguealready juggling vitamins, blood pressure meds, diabetes meds,
inhalers, or supplements. Adding one more item to the daily routine can feel like the straw that breaks the camel’s organizational system.
This is where small workflow fixes become surprisingly important: 90-day refills, syncing refill dates, using pill organizers, pharmacist check-ins,
and making the purpose of the medication crystal clear (“this lowers risk of heart attack/stroke over time”).
Experience #4: The “restart” story is more common than people think
Here’s an under-discussed experience: people stop a statin, worry about it for months, then eventually restartoften after a second conversation,
a follow-up lab, or a scare (like a family member’s cardiac event). The restart isn’t always dramatic. Sometimes it’s a quiet decision: “Okay, I’ll try a different one,”
or “Let’s do a lower dose,” or “I want to reduce my risk while I work on lifestyle changes.”
When clinicians normalize this pathway“it’s okay if we have to troubleshoot”patients often feel less trapped and more willing to try.
The experience shifts from “statin yes/no forever” to “risk reduction is a process,” which is usually the truth.
Taken together, these experiences explain why the 35% plateau is so stubborn. It’s not just about evidence. It’s about attention, trust, routines, and fear.
The good news is that these barriers are workable when healthcare systems and conversations are designed for humansnot just for guidelines.