Table of Contents >> Show >> Hide
- What TikTok Means by “Cortisol Face” (and Why That’s Not a Diagnosis)
- Cortisol 101: The Hormone TikTok Loves to Hate
- When High Cortisol Can Change Your Appearance: Cushing Syndrome and Steroid Medications
- Why Your Face Might Look Puffy (No “Cortisol Face” Required)
- Stress and Inflammation: The Real Connection TikTok Skips
- The Big Myth: “Fix Your Cortisol in 7 Days”
- A Reality-Based Checklist: What to Do If You’re Worried
- FAQs People Ask After Watching One Too Many “Cortisol Face” Videos
- Conclusion: Your Face Isn’t a Hormone Scorecard
- Experiences Related to “Cortisol Face”: What People Commonly Report (and What It Often Means)
- SEO Tags
If you’ve spent five minutes on TikTok lately, you’ve probably met the newest wellness boogeyman:
“cortisol face.” The videos usually follow a familiar scriptbefore-and-after photos,
a warning that your “puffy” face is proof your stress hormones are out of control, and a tidy list of
fixes (often paired with a link to buy something).
Here’s the problem: your face is not a mood ring for your cortisol. Stress can affect your body,
your skin, your sleep, and yes, even how “puffy” you might look sometimes. But TikTok often turns a real hormone
and a real medical condition into a vague aesthetic diagnosisand that’s where things go off the rails.
Let’s unpack what cortisol actually does, when it truly can change appearance, what “inflammation” really means,
and how to handle stress in a way that’s based on realitynot fear marketing.
What TikTok Means by “Cortisol Face” (and Why That’s Not a Diagnosis)
In most videos, “cortisol face” is described as a rounder-looking or puffy face,
sometimes with under-eye swelling, fuller cheeks, or a “bloated” look. The claim is that chronic stress raises cortisol,
and cortisol then causes facial swellingso your reflection becomes a stress report card.
But “cortisol face” is not a medical term. It’s a social-media label applied to a bunch of different things that can
look similar on camera: fluid retention, allergy swelling, sinus congestion, sleep deprivation, hormonal shifts, certain
medications, high-sodium meals, dehydration, or the way lighting and angles hit your face on a Tuesday.
The result? People start assuming they have a hormone disorder because their face looks different after:
finals week, a red-eye flight, a salty dinner, or a crying session over a sad movie (we’ve all been there).
Cortisol 101: The Hormone TikTok Loves to Hate
Cortisol isn’t “bad”it’s essential
Cortisol is a steroid hormone made by your adrenal glands. It helps regulate blood pressure, blood sugar,
metabolism, immune activity, and your body’s response to stress. In short: cortisol is part of why you can
get out of bed, handle a surprise pop quiz, and not pass out the moment something stressful happens.
Your cortisol has a daily rhythm
Cortisol typically follows a daily pattern (a circadian rhythm): it’s generally higher in the morning to help you wake up
and lower at night to support sleep. That’s one reason cortisol testing, when it’s medically needed, is done in specific ways
and at specific timesnot by vibes, selfies, or a “stress quiz” with a pastel background.
Stress can raise cortisolbut “stress” is a wide umbrella
Stress isn’t just one thing. There’s short-term stress (like public speaking) and long-term stress (like ongoing family conflict
or chronic sleep deprivation). Your body’s stress response involves multiple systemscortisol is one piece of the puzzle, alongside
adrenaline and the nervous system.
That’s why the TikTok storyline“stress equals cortisol equals swollen face”is too simplistic. Real biology is messier, slower,
and far less likely to fit into a 12-second montage with dramatic music.
When High Cortisol Can Change Your Appearance: Cushing Syndrome and Steroid Medications
There is a situation where excessive cortisol can contribute to a rounded or fuller-looking face. But it’s not the everyday
stress of school, work, or your group chat exploding at 2 a.m. It’s typically related to Cushing syndrome or
long-term use of corticosteroid medications.
Cushing syndrome: high cortisol as a medical condition
Cushing syndrome happens when the body is exposed to too much cortisol for a prolonged periodoften because of:
- Long-term corticosteroid medications (like prednisone), or
- Rare hormone-producing tumors that affect cortisol regulation.
Classic features can include a rounded face, weight gain concentrated in the upper body, skin changes (like easy bruising or stretch marks),
muscle weakness, high blood pressure, and blood sugar changes. It’s not subtleand it’s not diagnosed by appearance alone.
“Moon face” from steroids is realand it has context
The “moon face” people mention online is often linked to prolonged corticosteroid use. Steroids can cause fluid retention and changes in fat distribution.
If you’re prescribed steroids, do not stop them suddenly on your ownmedication changes should be supervised by a clinician.
Why everyday stress usually isn’t the culprit
Chronic stress can be harmful, but it usually doesn’t create the sustained cortisol exposure seen in Cushing syndrome.
Stress affects sleep, appetite, inflammation, and habits (hello, salty snacks and scrolling at midnight), which can
indirectly affect how your face lookswithout meaning you have a hormone disorder.
Why Your Face Might Look Puffy (No “Cortisol Face” Required)
Facial puffiness is commonand often temporary. Here are some of the most common, non-scary explanations:
Sleep and recovery (or lack of them)
Poor sleep can change fluid balance, increase under-eye swelling, and make skin look dull. Even one short night can show up on your face
the next dayespecially with dehydration or a high-sodium dinner.
Salt, hydration, and fluid shifts
Sodium affects water retention. Dehydration can also make your body hold onto fluid. Add heat, travel, or hormonal shifts, and your face can look different
from one day to the next. This is boring physiologyyet somehow TikTok made it a villain arc.
Allergies, sinus congestion, and irritation
Seasonal allergies, sinus issues, and skin irritation can cause swelling around the eyes and cheeks. If puffiness comes with itching, sneezing,
or watery eyes, cortisol is probably not the star of that show.
Medications and medical conditions
Some medications can cause swelling. Certain health conditions can, toolike thyroid issues, kidney problems, infections, or inflammatory reactions.
This is why persistent or worsening facial swelling deserves medical attention rather than a DIY supplement stack.
When facial swelling is a “don’t wait” moment
Seek urgent care if swelling is sudden and severe, involves lips or tongue, affects breathing, or comes with hivesthose can be signs of a serious allergic reaction.
If swelling lingers, worsens, or comes with other symptoms (unexplained weight changes, severe fatigue, high blood pressure, new stretch marks, or muscle weakness),
get evaluated by a healthcare professional.
Stress and Inflammation: The Real Connection TikTok Skips
Stress can influence inflammationbut not like a “face filter”
Stress affects the immune system and inflammatory signaling over time. Long-term stress can disrupt sleep, increase risk of unhealthy coping behaviors,
and affect immune function. But inflammation isn’t a single on/off switch, and it doesn’t reliably present as one specific face shape.
Stress can worsen certain skin conditions
If you’ve ever broken out right before a big event, you already know the stress-skin connection is real. Stress can aggravate conditions like acne, eczema,
psoriasis, and hives in some people. That’s not “cortisol face”that’s your skin responding to a complex mix of immune changes, barrier function, and behaviors
(like picking, skipping moisturizer, or sleeping in makeup because you’re exhausted).
Stress can affect collagen and skin appearance over time
Chronic stress can influence hormones and inflammatory pathways that may contribute to changes in skin quality over time. But that’s a slow, multifactor story
not a “you looked stressed for three days so your cheeks changed” situation.
The Big Myth: “Fix Your Cortisol in 7 Days”
Cortisol has a purpose. The goal isn’t to “eliminate” it or “detox” it. The goal is to support your body so the stress response isn’t constantly stuck in overdrive.
Beware the supplement shortcut
Social media often pushes supplements and powders that claim to “lower cortisol” or “flatten inflammation.” But supplements can have side effects,
interact with medications, and vary in quality. If someone’s selling you a solution that sounds like it was invented by a marketing team, take a breath.
“Natural” doesn’t automatically mean “safe” or “appropriate,” especially for teens and young adults.
Fear-based wellness content can backfire
When people start obsessing over facial “signs” of stress, it can increase anxietyironically worsening sleep and stress. That spiral doesn’t help your health,
and it definitely doesn’t help your relationship with your body.
A Reality-Based Checklist: What to Do If You’re Worried
If you’re concerned about facial puffiness and stress, try this grounded approach:
Step 1: Zoom out (literally and metaphorically)
- Did you sleep less than usual this week?
- Any allergy symptoms or sinus congestion?
- More salty foods than usual? Less water?
- New skincare products that could irritate your skin?
- Any new medications or dose changes?
Step 2: Support basics for 1–2 weeks
- Sleep: Aim for consistent sleep and wake times.
- Hydration: Drink enough water throughout the day.
- Balanced meals: Prioritize protein, fiber, and fruits/vegetables for steady energy.
- Movement: Gentle activity helps stress regulation (walks count).
- Stress outlets: Breathing exercises, journaling, music, stretching, or talking to someone you trust.
Step 3: Know when to get checked
Consider seeing a clinician if:
- Swelling is persistent, worsening, or painful.
- You have symptoms that don’t match “just stress” (like significant unexplained weight changes, muscle weakness, new purple stretch marks, high blood pressure, or blood sugar issues).
- You’re taking corticosteroids or have recently used them frequently.
- Swelling comes with breathing trouble, lip/tongue swelling, or hives (urgent).
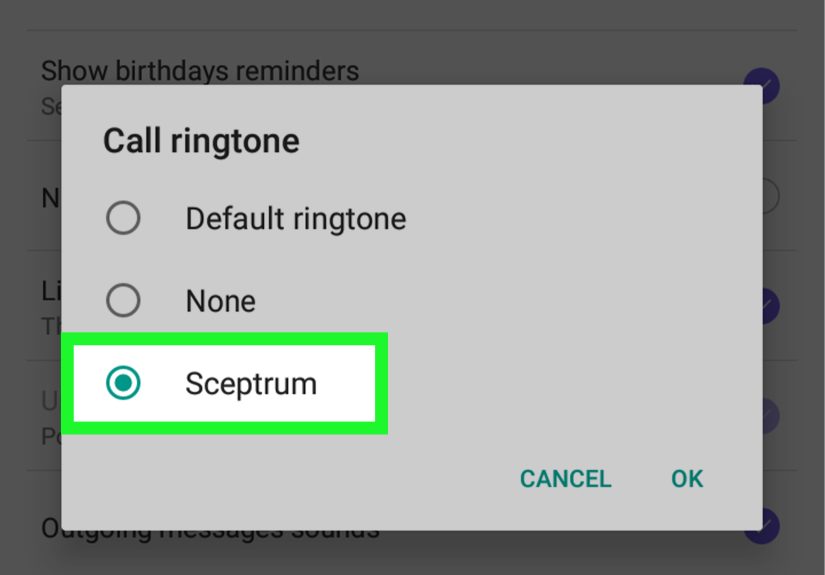
Step 4: If cortisol testing is needed, do it the medical way
Cortisol can be measured in blood, urine, or saliva, and interpretation depends on timing and context. When doctors evaluate high cortisol concerns,
they use structured testing strategiesnot a single random test and not a social-media checklist.
FAQs People Ask After Watching One Too Many “Cortisol Face” Videos
Is “cortisol face” real?
The phrase is a social-media label, not a diagnosis. However, true prolonged high cortisol from Cushing syndrome or long-term steroid use can cause a rounded face.
Most day-to-day puffiness has other explanations.
Can stress make your face puffy overnight?
Stress can disrupt sleep and habits, which can affect fluid retention. But overnight puffiness is more commonly linked to sleep, sodium, hydration, allergies, or irritation.
Does inflammation always show up on your face?
No. Inflammation is a broad biological process. Chronic inflammation is associated with many health conditions, but it doesn’t have one reliable “face shape.”
How do doctors treat Cushing syndrome?
Treatment depends on the cause. If steroids are involved, a clinician may taper them safely. If a tumor is involved, treatment could include surgery or medications.
This is specialized careand it’s why self-diagnosing from TikTok is risky.
Conclusion: Your Face Isn’t a Hormone Scorecard
TikTok didn’t invent cortisoland it definitely didn’t earn the right to diagnose you with it. Stress matters. Inflammation matters. Hormones matter.
But turning normal human variability into a scary diagnosis helps no one.
If you notice persistent swelling or symptoms that concern you, get medical guidance. If you’re simply feeling stressed and run down, start with the basics:
sleep, hydration, balanced meals, movement, and support. Those aren’t flashy. They don’t come in a pink tub with a scoop.
But they’re what actually move the needlewithout turning your face into a battlefield.
Experiences Related to “Cortisol Face”: What People Commonly Report (and What It Often Means)
Social media trends spread because they feel personal. Many people see the term “cortisol face” and think, “That’s me.”
Not because they’ve measured cortisolbut because they recognize the experience behind the videos: stress, exhaustion, and a body that feels off.
Below are common real-world scenarios people report, and the more likely explanations that fit what’s happening.
1) The “Exam Week” Face
A student hits a heavy weeklate-night studying, less water, more instant noodles, and sleep that’s basically a group project nobody agreed to.
In the mirror, their face looks puffier, especially around the eyes. They panic: “Is this cortisol face?”
In reality, the most likely drivers are sleep loss, sodium, and screen time (which can worsen the look of fatigue).
When that student returns to a normal routinebetter sleep, regular meals, hydrationthe puffiness often fades within days.
The lesson: the body is responsive. It doesn’t mean something is “broken.”
2) The “I’m Not Sick, It’s Just Allergies” Season
Some people report that “cortisol face” shows up every spring or fall. They wake up with puffy eyelids, pressure around the cheeks,
and a face that looks swollen on one side. They also have sneezing or itchy eyes but ignore those details because the TikTok label feels more dramatic.
This scenario often matches allergies or sinus congestion, not cortisol.
Addressing triggers, getting appropriate allergy care, and protecting the skin barrier can make a bigger difference than chasing cortisol-lowering hacks.
3) The Overworked, Under-Recovered Routine
Another common story comes from people juggling a packed schedule: school, work, family responsibilities, constant notifications,
and not enough downtime. They don’t necessarily feel “stressed” emotionally, but their body shows it: headaches, stomach discomfort,
breakouts, and a puffy look that comes and goes. What’s happening is often a blend of poor recoveryinconsistent sleep,
irregular meals, dehydration, and chronic tension. Stress physiology can contribute, but the best “fix” usually isn’t a supplement.
It’s boring (and effective) changes: a consistent bedtime, real meals, gentle movement, and a decompression habit that’s actually doable.
4) The Steroid Medication Surprise
Some people only discover the “moon face” concept after starting corticosteroids for a genuine medical reasonsevere asthma flare-ups,
autoimmune conditions, inflammatory bowel disease, or other issues. They notice facial fullness and feel self-conscious, especially when comments roll in.
This is one of the cases where appearance changes can be medication-related, and the right response is medical coordination:
discussing side effects, exploring the lowest effective dose, and never stopping abruptly without guidance. Many people report improvement as treatment plans
change or tapering occurs under supervision.
5) The Stress-Skin Connection That Actually Makes Sense
Finally, some people connect “cortisol face” to flare-upseczema patches, acne, redness, or hives that show up during stressful periods.
That connection can be real: stress can worsen inflammatory skin conditions for some individuals. But the “face” part is about skin inflammation
(and sometimes irritation from over-cleansing or trying too many products), not a single hormone reshaping the face overnight.
A calmer routinegentle cleanser, moisturizer, sunscreen, fewer actives, and stress supportoften does more than aggressive “detox” approaches.
Across these experiences, one theme stands out: people want a simple explanation for a complicated season of life.
TikTok hands them a catchy label. But your body usually needs something else: rest, consistency, andwhen symptoms persistprofessional evaluation.
If the trend leaves you feeling anxious or hyperfocused on your appearance, that’s a sign to step back. Health is not a face shape.