Table of Contents >> Show >> Hide
- Estrogen 101: The Main Types (E1, E2, E3) and What They Do
- Why an Estrogen Test Might Be Ordered
- What Exactly Is an “Estrogen Test”?
- How to Prepare for an Estrogen Test
- What Happens During the Test: Step-by-Step
- Understanding Your Results (Without Spiraling at 2 A.M.)
- What High or Low Estrogen Results Can Mean (Examples, Not Diagnoses)
- Accuracy Notes: Things That Can Mess With Estrogen Testing
- Frequently Asked Questions
- Real-World Experiences: What Estrogen Testing Often Feels Like (About )
- Conclusion
- SEO Tags
Estrogen gets labeled as “the female hormone,” which is a little like calling electricity “the lamp ingredient.”
It’s technically involved, but it’s also doing a whole lot more behind the scenesand it matters in all bodies.
Estrogen helps coordinate reproduction and puberty, yes, but it also plays roles in bone strength, brain signaling,
skin and connective tissue, cholesterol patterns, and more.
So when a clinician orders an estrogen test, they’re not just “checking hormones” in the vague, meme-y sense.
They’re trying to answer a specific question: Is your body making the right type of estrogen, at the right time,
in the right amount, for what’s going on right now?
Estrogen 101: The Main Types (E1, E2, E3) and What They Do
“Estrogen” isn’t one single hormone. It’s a group. The three you’ll see most often on lab reports are:
- Estradiol (E2): Usually the “star player” during the reproductive years. It rises and falls across the menstrual cycle.
- Estrone (E1): Often becomes the more dominant estrogen after menopause. It’s made in several tissues, including fat tissue.
- Estriol (E3): Most associated with pregnancy, because it’s produced in much larger amounts during pregnancy.
Estrogen’s jobs change depending on age and life stage. During puberty, it supports development. During cycling years,
it helps coordinate ovulation and the uterine lining. During and after menopause, lower estrogen can contribute to
symptoms like hot flashes and bone density changes. In males, estrogen is present too, and it supports bone health
and is part of the normal hormone “balance” with testosterone.
Why an Estrogen Test Might Be Ordered
Estrogen testing is usually done to investigate symptoms, monitor certain treatments, or help diagnose conditions
that affect the ovaries, testes, pituitary gland, adrenal glands, or placenta (during pregnancy).
1) Menstrual cycle changes and fertility evaluation
Because estradiol changes across the cycle, testing can help evaluate ovarian function and sometimes supports fertility workups.
For example, clinicians may check estradiol alongside other hormones (like FSH and LH) early in the cycle to better understand
how the ovaries are responding.
2) Puberty timing and development
If puberty seems unusually early or delayed, estrogen testing may be part of a broader evaluation, often paired with other labs
and growth/development history.
3) Menopause and perimenopause questions
This is where things get tricky: in perimenopause, hormone levels can swing dramatically from week to week.
Many clinicians diagnose perimenopause primarily by age, symptoms, and menstrual patternnot by a single hormone test.
Estrogen tests can still be useful in certain situations, but they’re not always the “final answer” people hope for.
4) Possible hormone-producing tumors or endocrine disorders
Very high (or unexpectedly low) estrogen levels can sometimes signal a condition affecting hormone-producing organs.
Testing is used as one clue among manysymptoms, physical exam, imaging, and additional labs.
5) Pregnancy-related monitoring
Estriol is especially relevant during pregnancy. It may be measured as part of certain prenatal screening strategies,
because it reflects placental and fetal contributions to hormone production.
6) Male hormone balance concerns
In males, estradiol may be checked when there are signs of estrogen excess or imbalance (for example, certain breast tissue changes),
or to evaluate some endocrine conditions.
What Exactly Is an “Estrogen Test”?
“Estrogen test” can mean a few different things. Your clinician might order one specific estrogen (most commonly estradiol/E2),
or a broader measurement depending on the clinical question.
Common estrogen-related lab orders
- Estradiol (E2), serum (blood): The most common estrogen blood test.
- Estrone (E1), serum: Sometimes used in evaluations involving menopause status or estrogen production patterns.
- Estriol (E3), blood or urine: Most relevant during pregnancy, and sometimes ordered as a 24-hour urine test.
- Total estrogens: A combined measure (less common than a targeted estradiol test).
Blood vs. urine vs. saliva: what’s the difference?
Blood testing is the standard in most clinical settings because it’s widely available and generally reliable.
Urine testing may be used for certain estrogen measurements (including some estriol assessments),
often as a 24-hour collection.
Saliva testing exists (including some at-home options), but results can be harder to interpret,
and many clinicians prefer blood/urine for medical decision-makingespecially in pregnancy.
How to Prepare for an Estrogen Test
Preparation depends on which estrogen is being tested and why.
Many people don’t need to fast. The most important “prep” is giving your clinician the right context.
Tell your clinician about medications and supplements
Share a list of anything that could influence hormone levels or lab accuracy, including:
- Birth control or hormone therapy
- Fertility medications (if applicable)
- Androgens, anti-androgens, or endocrine-related medications
- Biotin (a common hair/skin/nails supplement) because it can interfere with certain lab assays
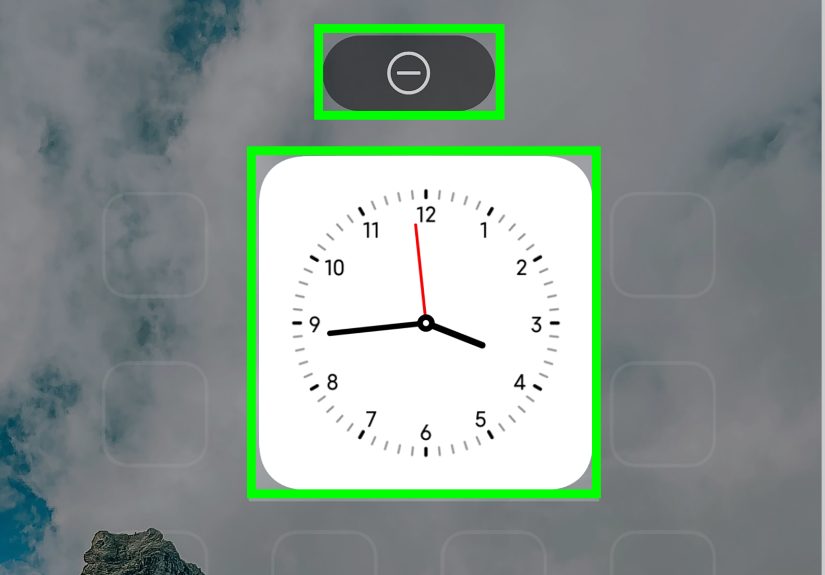
Timing can matter (especially for estradiol)
If you menstruate, your clinician may request testing on a specific cycle dayoften early in the cycle for certain evaluations.
If you don’t have periods or your cycles are irregular, the timing may be more flexible, and interpretation will lean more heavily
on symptoms and other labs.
What Happens During the Test: Step-by-Step
Blood test (most common)
- You check in at a clinic or lab.
- A technician cleans the skin and draws blood from a vein (usually in the arm).
- The sample is labeled and sent for analysis.
- You go about your dayno special “recovery time” required for most people.
Common minor side effects: brief pain at the needle site, a small bruise, or lightheadedness.
Serious complications are uncommon.
24-hour urine collection (often used for certain estriol testing)
- You’ll receive a container and instructions from the lab.
- You collect all urine over a full 24-hour period (yes, it’s a commitment).
- You store the container as directed (often in a cool place) and return it promptly.
This approach can provide a more complete picture of hormone output over time, but it only works if the collection is done carefully.
Missed samples can throw off results.
Saliva testing
Saliva tests typically involve collecting a spit sample at home. They may be marketed for “hormone balance,”
but interpretation can be challenging, and clinical decisions often rely on blood/urine results instead.
Understanding Your Results (Without Spiraling at 2 A.M.)
First: breathe. An estrogen number is not a personality test. It’s a snapshot.
And estrogen is famous for changing depending on age, cycle timing, pregnancy status, and medications.
Why “normal range” is a moving target
- Different labs use different reference ranges and testing methods.
- Estradiol varies across the menstrual cyclea lot.
- Life stage matters (puberty, cycling years, pregnancy, menopause).
- Context matters: symptoms, other hormones, and medical history shape interpretation.
Typical patterns clinicians look for
Instead of chasing one “perfect” number, clinicians look for patterns that match (or don’t match) what your body should be doing.
Here are examples of the kinds of patterns they may consider:
- Lower estradiol than expected might be seen with decreased ovarian function, certain pituitary signaling problems, or after menopause.
- Higher estradiol than expected can occur in pregnancy, during certain fertility treatments, or in some hormone-producing conditions.
- Estrone dominance may be more common after menopause (and may be influenced by body composition and metabolism).
- Estriol changes are especially relevant during pregnancy and are interpreted within that context.
A practical “how to read the report” checklist
- Confirm which estrogen was tested: E1, E2, E3, or total estrogens.
- Check the units: commonly pg/mL for estradiol, but reports vary.
- Look at the lab’s reference interval on your report (don’t rely on random charts online).
- Note your timing and status: cycle day, pregnancy status, menopause status, medications.
- Interpret alongside other labs your clinician ordered (often FSH, LH, progesterone, testosterone, prolactin, TSH).
What High or Low Estrogen Results Can Mean (Examples, Not Diagnoses)
Estrogen results are best treated like clues in a mystery. A clue can point you in a directionbut it can’t solve the whole case alone.
Here are some real-world examples of how results may be used.
If estradiol (E2) is lower than expected
- Example: Someone with missed periods and hot-flash-like symptoms may have low estradiol plus high FSH, suggesting the ovaries aren’t responding as expected.
- Example: A teen with delayed puberty may have low estradiol, prompting a broader evaluation of pituitary and ovarian signaling.
- Example: Postmenopause, low estradiol is expected and often aligns with symptom patterns and bone-health considerations.
If estradiol (E2) is higher than expected
- Example: During pregnancy, estradiol levels rise substantiallycontext is everything.
- Example: In fertility treatment monitoring (where applicable), estradiol can rise quickly as follicles develop.
- Example: Unexpectedly high estradiol in someone not pregnant and not using hormones may lead a clinician to look for medication effects, lab interference, or less common endocrine causes.
If estriol (E3) is the focus
Estriol is most meaningful in pregnancy-related testing. It’s typically interpreted as part of a broader prenatal screening picture,
not as a standalone “good” or “bad” result.
Accuracy Notes: Things That Can Mess With Estrogen Testing
Biotin interference (the sneaky supplement problem)
High-dose biotin supplements can interfere with certain lab tests and cause results that look “off” even when your body is doing the same thing it did yesterday.
If you take biotin, tell your clinician and the lab. They may recommend pausing it before testing, depending on the assay.
Timing and variability
Estrogen isn’t steady like a speed limit signit’s more like traffic. It changes over the day, over the month, and across life stages.
That’s why clinicians sometimes repeat testing, pair it with other hormones, or focus on symptoms rather than chasing a single number.
At-home hormone tests
Some at-home tests can provide useful information, but they can also create confusion if the result is treated like a diagnosis.
If you use an at-home test, bring the results to a clinician who can interpret them in context and, if needed, confirm with clinical-grade testing.
Frequently Asked Questions
Do I need an estrogen test to “prove” perimenopause?
Often, no. Perimenopause is commonly diagnosed based on symptoms and menstrual changes because hormone levels can swing widely.
Testing may be used in specific situations, but it’s not always required to move forward with a plan.
Can I “balance estrogen” with detoxes or quick fixes?
If you see a product promising to “reset your hormones in 7 days,” treat it like a timeshare pitch: smile, back away slowly.
Estrogen balance is influenced by multiple organs and systems, and meaningful changes usually come from medical evaluation
(when needed), evidence-based treatment, and long-term health habitsnot miracle teas.
What should I do if my result is outside the reference range?
The next step is usually discussionnot panic. Bring the report to the clinician who ordered it.
Ask what the number means for your situation, whether timing or supplements could have affected it, and whether follow-up testing is needed.
Real-World Experiences: What Estrogen Testing Often Feels Like (About )
People don’t usually walk into an estrogen test feeling casually curious, like they’re browsing paint swatches.
More often, they’re walking in with a question that’s been living rent-free in their brain:
“Is what I’m feeling normal?” Here are a few common, realistic snapshots of what the experience can look like.
(These are composite scenariosmeant to reflect typical experiences, not any one person’s story.)
Scenario 1: “We’re testing on cycle day 3… wait, which day is day 1?”
A lot of people get estrogen testing as part of a bigger hormone panel early in the cycle. The instructions can feel oddly intense:
pick a specific day, schedule the lab, and show up in a small windowwhile life continues to do life things.
It’s common to double-check the calendar three times, then text a friend like, “Is day 1 the first day of my period, or the first day I notice it?”
(Typically, clinicians mean the first day of full flow.) The blood draw itself is quick. The emotional part is the waiting
especially if the test is tied to fertility questions or months of unpredictable cycles.
Scenario 2: “My symptoms are loud, but my labs look ‘fine’now what?”
This is one of the most frustrating experiences: you finally get tested, and the result lands inside the reference interval.
Some people feel relief; others feel dismissed. But estrogen is a moving target, especially during perimenopause.
A “normal” value on a Tuesday morning doesn’t automatically cancel out real symptoms.
In these cases, a good follow-up conversation is everything: What was the clinical question? Was timing important?
Are other hormones relevant? Is the plan based on symptoms, trend over time, or additional evaluation?
Many people leave that appointment feeling better not because they got a dramatic numberbut because they got a clear plan.
Scenario 3: The surprise variablesupplements
Plenty of people take a hair/skin/nails supplement without thinking twice. Then they hear, “Are you taking biotin?”
and realize their “simple lab test” has a plot twist. If the clinician suspects assay interference, they may recommend stopping biotin
for a short period and repeating the test. That can feel annoying (nobody wants extra needle pokes),
but it’s also empowering: it means a weird result might not reflect your body at allit might reflect the chemistry of the test.
People often remember this lesson forever: before labs, list everything you take, even the “harmless” stuff.
Scenario 4: “I didn’t expect the test to be emotional.”
Hormone testing can hit deeper than people expect. If you’re 16 and being evaluated for delayed puberty, it can feel awkward and vulnerable.
If you’re 42 and your body feels unfamiliar, it can feel scary. If you’re 55 and trying to protect your bones and quality of life,
it can feel urgent. The lab experience is usually routine, but the meaning isn’t.
One of the most helpful coping tools is to write down your questions before the appointment:
“What does this test answer?” “What can’t it answer?” “If it’s high/low, what happens next?”
That turns the experience from “waiting for a verdict” into “gathering information.”
In the end, estrogen testing is most useful when it’s part of a bigger pictureyour symptoms, your history, your life stage,
and (importantly) a clinician who can translate numbers into next steps. The goal isn’t a perfect number.
The goal is understandingand a plan that actually helps you feel better.
Conclusion
Estrogen hormones are part of a complex, well-choreographed systemexcept sometimes the choreography goes off-script,
and that’s when estrogen testing can be helpful. Whether the test is measuring estradiol (E2), estrone (E1), estriol (E3),
or a broader estrogen level, the key is context: cycle timing, life stage, medications, supplements, and symptoms all shape what the result means.
If your number is high, low, or confusingly “normal,” the smartest next move is a conversation with a clinician who can interpret it as part of the whole story.