Table of Contents >> Show >> Hide
- What Is “Fart Walking,” Exactly?
- Why You Feel Bloated (And Why Walking Might Help)
- What the Science Says About Fart Walking for Gas and Bloating
- The Blood Sugar Bonus: Why Post-Meal Walking Got Real Attention
- Will Fart Walking Help With Constipation, Too?
- How to Do a Fart Walk (Without Overthinking It)
- Common Myths (and Mistakes) About Fart Walking
- When Fart Walking Might Not Be Enough (and When to Get Checked)
- Other Smart, Science-Backed Ways to Reduce Gas and Bloating
- So… Does Fart Walking Work?
- Experiences: What a “Fart Walk” Really Feels Like (A 7-Day, Real-World Look)
- Conclusion
TikTok has turned everything from “sleepy girl mocktails” to “hot girl walks” into a lifestyle. Now it has gifted the internet
a phrase that is both hilarious andannoyinglypretty practical: fart walking.
The concept is exactly what it sounds like: you take a short stroll after eating, and, well… your body handles the rest.
It’s not glamorous. It’s not subtle. But it might be one of the more realistic wellness trends to come out of a social feed
full of chlorophyll water and “what I eat in a day” fantasies.
So does fart walking actually work for digestive healthor is it just a catchy name for something your grandparents
already did (minus the branding)? Let’s break down what’s happening in your gut, what research suggests about movement after meals,
and how to do it without turning your neighborhood into a crime scene.
What Is “Fart Walking,” Exactly?
Fart walking is a short, easy-paced walk taken after a mealusually within about an hour, often for
5 to 15 minutes. The goal isn’t training for a marathon. It’s gentle movement that may help your digestive system
move food and gas along, reduce that tight “balloon belly” feeling, and even blunt post-meal blood sugar spikes.
The term got popular because it’s funny (obviously), but the habit behind itpost-meal walkinghas been recommended
for ages in many cultures. TikTok didn’t invent the walk. TikTok just named it in a way nobody can un-hear.
Why You Feel Bloated (And Why Walking Might Help)
First, a reality check: gas is normal. Everyone produces it. Some people just have a more dramatic relationship with it.
Bloating can be caused by swallowing air (hello, eating fast), gas produced by gut bacteria during digestion, constipation, certain foods,
and sometimes underlying digestive conditions.
The “Gas Math” Your Body Does All Day
Gas in your digestive tract generally comes from two main sources:
- Air you swallow while eating, drinking, chewing gum, or chugging carbonated drinks.
- Fermentation as gut bacteria break down certain carbohydrates (beans and lentils, we’re looking at you).
Your body gets rid of gas by belching, passing gas, and absorbing some of it into the bloodstream. When that process slows down,
gas can feel “stuck,” causing pressure and discomfort.
Movement = A Gentle Nudge for Your Gut
Walking doesn’t “shake loose toxins” or do anything mystical. It’s simpler: light activity can support
gastrointestinal motilitythe wave-like muscle contractions (peristalsis) that move contents through your intestines.
Think of it as giving your digestive tract a polite tap on the shoulder: “Hey buddy, whenever you’re ready.”
When you walk, your abdominal muscles and diaphragm move, your posture changes, and your nervous system shifts into a rhythm that may help
food and gas travel more smoothly. For many people, that means less bloating and easier gas releaseoften without the intense emotional journey
of lying on the floor doing knee-to-chest yoga poses in the middle of the living room.
What the Science Says About Fart Walking for Gas and Bloating
There isn’t a huge body of research specifically labeled “fart walking” (shocking, I know). But there is research on
mild physical activity and walking after meals for bloating and gas-related symptoms.
Evidence That Mild Activity Can Help Gas Clearance
Studies have found that mild physical activity can enhance intestinal gas clearance and reduce symptoms in people who feel bloated.
The takeaway: being gently active may help your body move gas through and out more efficiently.
Post-Meal Walking and “Functional Bloating”
Functional abdominal bloating (bloating without a clear structural cause) is common. A randomized clinical trial compared short post-meal activity
with other approaches and found improvements in symptoms like bloating, belching, and discomfort with minimal exercise after meals.
This doesn’t mean walking is a cure-all, but it supports the idea that a low-effort habit can have real comfort benefits for some people.
Translation: It’s Not MagicIt’s Mechanics
If you tend to feel puffy and uncomfortable after dinner, a short walk may:
- encourage your gut to keep moving instead of “parking” your meal for the night,
- reduce the sensation of trapped gas,
- support regularity (especially if constipation plays a role),
- lower the odds that you end your meal by unbuttoning your jeans like a Victorian fainting scene.
The Blood Sugar Bonus: Why Post-Meal Walking Got Real Attention
Here’s where fart walking goes from funny to legitimately useful: research suggests that
light movement after meals can reduce post-meal blood sugar spikes.
After you eat, glucose rises in your bloodstream. Your body responds by releasing insulin so your cells can use that glucose for energy.
A gentle walk helps your muscles use glucose, potentially lowering the peak.
How Little Walking Are We Talking?
Multiple analyses have found benefits from very short bouts of activitysometimes just a few minutesespecially when done
soon after eating. You don’t need to turn dinner into a triathlon. You need movement that’s easy enough to do consistently.
Who Might Benefit Most?
Post-meal walking can be especially relevant for:
- People with prediabetes or insulin resistance
- People with type 2 diabetes (especially for managing post-meal glucose)
- People with sedentary jobs who want a low-barrier habit
- Basically anyone who wants a tiny health win that doesn’t require equipment, a membership, or emotional courage
If you take glucose-lowering medication (especially insulin or drugs that can cause hypoglycemia), it’s smart to talk with your clinician about timing and safety.
Even gentle movement can change glucose dynamics for some people.
Will Fart Walking Help With Constipation, Too?
It can. Not always, and not instantly, but walking is commonly recommended as part of a constipation-friendly lifestyle because movement supports
overall gut motility and routine.
If your “bloating” is partly a traffic jam problemslower transit, incomplete bowel movements, irregularitythen daily walking (including short post-meal strolls)
may help over time, especially alongside hydration and adequate fiber.
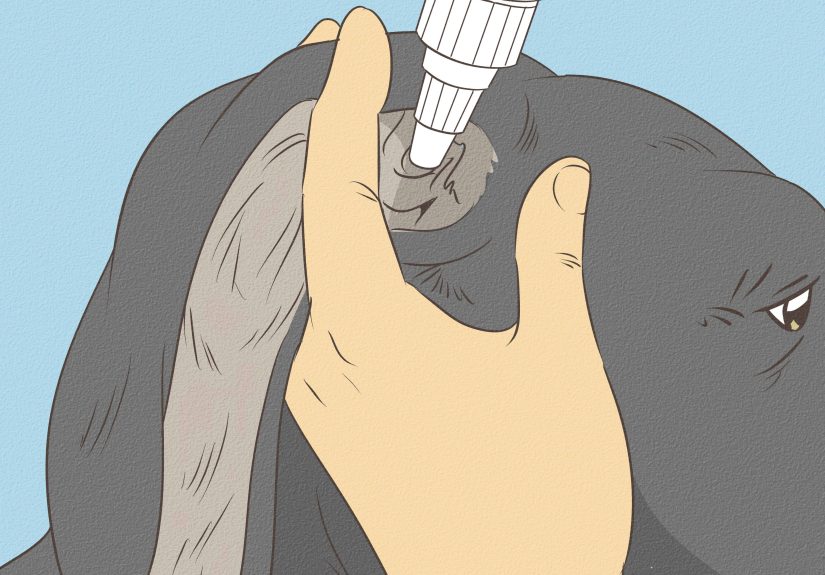
How to Do a Fart Walk (Without Overthinking It)
The best fart walk is the one you’ll actually do. Here’s a simple formula that works for most people.
1) Timing: Aim for Within 10–60 Minutes After Eating
You don’t have to sprint out the door with a napkin still tucked into your shirt. But walking fairly soon after a meal is the point.
Many people find 10–20 minutes after finishing is a sweet spotespecially after dinner.
2) Duration: 5–15 Minutes Is Plenty
TikTok loves extremes. Your gut does not. A short walk is enough to get benefits without provoking nausea or cramps.
You can always do longer if it feels good, but “short and consistent” beats “long and never.”
3) Intensity: Keep It Easy
Use the talk test: you should be able to hold a conversation without sounding like you’re being chased.
The goal is gentle movement, not a digestive stress test.
4) Route Options for Real Life
- Apartment loop: hallway laps or stairs at a relaxed pace
- Indoor “kitchen circuit”: pace while cleaning up or making tomorrow’s lunch
- Neighborhood block: a simple out-and-back with a podcast
- Social version: walk with a partner (and agree on the “no commentary” policy)
5) Make It More Digestive-Friendly
- Stand tallslouching can compress your abdomen and make you feel more “stuffed.”
- Breathe slowly through your nose if possible; it can reduce air swallowing.
- Avoid guzzling carbonated drinks right before you go.
Common Myths (and Mistakes) About Fart Walking
Myth: “If a little helps, a fast power walk is better.”
Not necessarily. High-intensity exercise right after a big meal can make some people feel nauseated or crampy. Start easy.
If you want a harder workout, save it for later.
Myth: “It cures IBS.”
Walking may help some IBS symptoms for some people, but IBS is complex and individualized. If you have persistent symptoms,
you’ll likely need a broader plan (dietary triggers, stress management, medical guidance, and sometimes medication).
Mistake: Expecting instant perfection
Some walks will be wildly productive. Some will be uneventful. That’s normal. The win is building a habit that supports digestion and metabolic health over time.
When Fart Walking Might Not Be Enough (and When to Get Checked)
Occasional gas and bloating are normal. But if bloating is frequent, severe, or paired with other symptoms, it’s worth getting medical guidance.
Consider reaching out to a healthcare professional if you notice:
- unexplained weight loss,
- blood in stool or black/tarry stools,
- persistent vomiting,
- severe abdominal pain,
- new or worsening symptoms that don’t improve with basic changes,
- bloating that is constant or progressively worsening.
Other Smart, Science-Backed Ways to Reduce Gas and Bloating
Fart walking is a good toolbut it’s not the whole toolbox. If you want fewer “why do I feel like a parade float?” days, combine walking with these practical habits:
Slow Down When You Eat
Eating quickly increases swallowed air and makes it easier to overeat. Chew thoroughly, pause between bites, and try not to treat lunch like a timed competition.
Audit Carbonation and Gum
Carbonated drinks add gas. Chewing gum can increase swallowed air. If bloating is a frequent issue, those are easy places to experiment.
Track Trigger Foods (Gently, Not Obsessively)
For some people, certain foods are frequent culprits: beans, lentils, onions, garlic, certain dairy products (if lactose intolerant),
sugar alcohols, and high-FODMAP foods. You don’t have to ban everythingjust notice patterns.
Support Regularity
If constipation is involved, daily movement helps, but hydration and fiber matter too. Increase fiber gradually and pair it with enough fluids.
OTC Options Can Help Sometimes
Some people find occasional relief from simethicone (for gas bubbles) or targeted approaches depending on the cause.
If you’re needing OTC products frequently, it’s worth reviewing the bigger picture with a clinician.
So… Does Fart Walking Work?
For many people, yesat least in the ways that matter most:
less post-meal bloating, easier gas passage, and better post-meal blood sugar control.
It’s not a miracle. It won’t erase every digestive issue. But it’s low-risk for most people, it’s free, and it’s surprisingly effective for something that sounds like a prank.
If nothing else, fart walking is a rare wellness trend that doesn’t demand supplements, suffering, or a complicated identity shift.
It’s just you, a sidewalk, and your digestive system doing paperwork.
Experiences: What a “Fart Walk” Really Feels Like (A 7-Day, Real-World Look)
Since I can’t follow you around with a clipboard (and you definitely don’t want that), the best way to describe fart walking “results”
is to summarize the kinds of experiences people commonly reportespecially when they stick with it for a week.
Consider this a realistic preview, not a promise. Bodies vary, meals vary, and sometimes your gut simply chooses chaos.
Day 1: The Awkward Discovery Phase
Many first-timers report the same thing: “Oh… this is just a normal walk.” The only difference is you’re paying attention to your stomach.
After dinner, the first few minutes can feel slightly heavyespecially if you ate fast or had a large meal. Then, somewhere around minute five,
you may notice less pressure. Sometimes nothing happens at all. Sometimes your body decides to be extremely efficient and you learn why the trend has that name.
The biggest surprise for most people is how quickly the post-meal “brick in the belly” sensation can ease with gentle movement.
Day 2: The “I Slept Better?” Effect
A common report: the walk helps people feel less reflux-y or overfull when they go to bedparticularly after a heavy dinner.
The walk isn’t a cure for heartburn, but avoiding a straight-to-couch collapse can make bedtime feel more comfortable.
People who tend to snack at night also notice something interesting: walking creates a natural “meal is done” boundary.
It’s not willpowerit’s a routine that signals closure.
Day 3: The Portion Reality Check
Around day three, the walk becomes a feedback system. If you eat a meal that’s greasy, huge, or gas-triggering, the walk may feel slower and more sluggish.
If you eat a balanced meal and take an easy stroll, you may feel lighter faster. Many people say fart walking doesn’t just reduce bloatingit makes them
more aware of which foods reliably set off discomfort. It’s like your gut sends a push notification: “We need to talk about that second helping.”
Day 4: The Office-Friendly Version
People who try fart walking after lunch often adapt it for real life: a lap around the building, a few minutes pacing while on a call,
or walking to refill water instead of staying glued to a chair. The big win here is consistency. A short walk is easy to repeat, and repetition is where the
blood-sugar and digestion benefits tend to stack. Bonus: it’s a decent mental reset between tasks.
Day 5: The “Where Did My Afternoon Crash Go?” Moment
Some people notice less post-lunch sleepiness when they walk afterward. That’s not guaranteedsleep, stress, and meal composition play major roles
but light activity can make the afternoon feel steadier. If you usually get a heavy slump after carb-heavy meals, a short walk can feel like a gentle brake
on that roller coaster.
Day 6: The Social Test
Doing the walk with a friend or partner is where the habit either becomes permanent or dies of embarrassment.
Couples often create unofficial rules: no teasing, no commentary, and if something happens… we pretend we’re birdwatching and keep moving.
The upside is accountability. The walk becomes a mini ritual: a decompression moment, a check-in, and a simple way to move more without scheduling a workout.
Day 7: The Habit Clicks (Or You Customize It)
By the end of a week, many people settle into a personalized version: maybe only after dinner, maybe after the biggest meal, maybe just on bloat-prone days.
The most common “sticky” benefits people mention are feeling less stuffed, fewer nights of lying down uncomfortably full, and a sense that digestion feels more
predictable. The trend’s secret is that it’s not about perfection. It’s about a small nudgedone often enough to matter.
If you try it and feel worsecramps, nausea, worsening refluxscale back intensity, shorten the duration, or shift the timing.
And if bloating is persistent or severe, treat fart walking as a supportive habit, not a diagnosis or a solution.
Conclusion
Fart walking has the comedic branding TikTok loves, but the habit underneath it is refreshingly sensible: a short, gentle post-meal walk can support
digestion, help move gas along, and reduce post-meal blood sugar spikes for many people. It’s not a cure for chronic digestive disorders, and it won’t make
every meal consequence-free. But it’s easy, low-cost, and surprisingly effective for something with such an unserious name.
If you want a gut-friendly habit that doesn’t require a blender, a supplement stack, or a personality overhaul, this might be the most realistic trend
you’ll see all year. Just remember: the goal is comfort and consistencynot speed, suffering, or turning your evening stroll into a competitive sport.