Table of Contents >> Show >> Hide
- What Happened in the Assurance IQ Case?
- What Did the FTC Say Assurance IQ Did Wrong?
- How the $100 Million Judgment Works
- Why This Case Matters Beyond Assurance IQ
- Lessons for Consumers Shopping for Health Insurance Online
- Compliance Takeaways for Marketers and Insurtechs
- Real-World Experiences and Scenarios Around the Assurance IQ Model
- Conclusion: A Landmark Case in Digital Health Insurance Marketing
When a federal regulator drops a $100 million judgment on your business, that’s not just a slap on the wristthat’s the regulatory equivalent of a meteor strike. In 2025, the Federal Trade Commission (FTC) secured a $100 million judgment against Assurance IQ, an insurtech company once hailed as a digital-disruption darling in the health insurance space. The case centered on how Assurance marketed health insurance plans online and through telemarketingand what consumers were actually getting once they enrolled.
If you’ve ever tried to buy health insurance online and ended up buried under calls, pop-ups, and fine print, this case will feel eerily familiar. The FTC’s action isn’t just about one company; it’s a warning shot to the entire lead generation, insurtech, and online insurance marketing ecosystem.
What Happened in the Assurance IQ Case?
The short version
The FTC alleged that Assurance IQ misled consumers by pitching health plans as if they offered comprehensive coverage“like ACA plans”when many of them were not comprehensive at all. Instead, consumers often ended up in short-term medical or limited-benefit plans with significant gaps, exclusions, and caps on coverage. Thousands of people thought they were fully protected, only to discover big out-of-pocket bills later.
To resolve these allegations, Assurance IQ agreed to a settlement featuring a $100 million monetary judgment and a permanent injunction setting strict rules on how it (and related entities) can market health insurance going forward. That $100 million forms the bulk of a broader $145 million package, with the remaining $45 million coming from another company involved in the same lead-generation ecosystem, MediaAlpha.
Who is Assurance IQ, and how did we get here?
Assurance IQ started out as a fast-growing insurtech platform promising to match consumers with health and financial products using data-driven technology and online tools. Its success caught the eye of traditional insurance giant Prudential Financial, which acquired Assurance IQ in 2019 for about $2.35 billion.
The idea was simple: combine Prudential’s product lineup and financial strength with Assurance’s direct-to-consumer digital platform. In theory, it was a perfect marriage of old-school insurance and new-school tech. In practice, the regulatory and compliance risks of aggressive health insurance marketing turned out to be far bigger than anyone expected.
By 2024, Prudential had announced it would shut down Assurance after massive goodwill write-downs and operational challenges. The FTC case was, in many ways, the final chapter: a detailed federal complaint and a nine-figure settlement over how Assurance’s marketing and telemarketing practices treated consumers.
What Did the FTC Say Assurance IQ Did Wrong?
According to the FTC, this was not a case of one or two stray misstatements. The agency alleged a systematic pattern of deceptive practices spanning online funnels, TV ads, telemarketing scripts, and lead-generation partnerships.
Misrepresenting coverage as “comprehensive”
One of the most serious allegations: Assurance IQ and its agents allegedly told consumers that the plans they were buying offered coverage comparable to Affordable Care Act (ACA) plans“comprehensive” protection with essential health benefits like hospitalization, maternity care, and prescription drugs. In reality, many of the products were:
- Short-term medical plans with major exclusions and limits,
- Limited-benefit indemnity plans that pay only a small fixed amount per service, and
- Supplemental products such as discount cards and telemedicine add-ons that do not replace comprehensive insurance.
Consumers were allegedly told that preexisting conditions were covered, that there were no caps on doctor visits, or that networks were broadclaims the FTC said were false or seriously misleading.
Flooding consumers with telemarketing and robocalls
The FTC also highlighted aggressive telemarketing tactics. Consumers who submitted information onlineoften believing they were getting quotes for comprehensive coveragefound themselves bombarded with calls. These calls, sometimes automated, allegedly went far beyond what consumers reasonably consented to and violated the Telemarketing Sales Rule (TSR).
In effect, a consumer’s request for information became a digital “open season” signal for calls and pitches. Regulators described it as a deceptive lead-generation machine built on relentless outreach and incomplete disclosure.
Violations of the FTC Act and Telemarketing Sales Rule
The FTC’s complaint alleged that Assurance IQ’s conduct violated:
- Section 5 of the FTC Act, which prohibits unfair or deceptive acts or practices; and
- The Telemarketing Sales Rule (TSR), which sets consent, disclosure, and recordkeeping requirements for telemarketing campaigns.
When you mix misleading sales scripts with high-pressure outbound calls to vulnerable consumerspeople trying to find affordable health coveragethe FTC tends to respond quickly and decisively. This case is a textbook example.
How the $100 Million Judgment Works
The headline number is clear: $100 million tied specifically to Assurance IQ. But what does that actually mean in practice?
Money earmarked for consumer refunds
The $100 million judgment is designed primarily to fund consumer redress. The FTC has indicated that the combined $145 million from Assurance IQ and MediaAlpha will be used to refund consumers who were misled into buying health insurance products that did not deliver the promised coverage.
While not every consumer will necessarily receive a refundthese programs usually depend on available records, claims, and administrative processesthe scale of the fund signals how widespread the agency believes the harm was.
Permanent injunction and strict marketing rules
The settlement also includes a permanent injunction, which is legal shorthand for “you’re not allowed to do this again, ever, and here are the rules you must follow from now on.” Among other things, the order:
- Prohibits misrepresentations about the nature, coverage, and limitations of health plans,
- Requires clear and conspicuous disclosures when products are not comprehensive or ACA-compliant,
- Imposes strict consent, documentation, and recordkeeping obligations for telemarketing and lead generation, and
- Mandates ongoing compliance, monitoring, and reporting to the FTC.
For any future business models tied to Assurance or its successors, the message is simple: no more “trust us, you’re fully covered” marketing unless the paperwork and reality fully back that up.
Why This Case Matters Beyond Assurance IQ
The FTC did not treat this as a one-off mistake by a single insurtech startup. Instead, the agency framed it as part of a broader crackdown on deceptive online health insurance marketing and lead generation.
A warning to the lead-generation ecosystem
Assurance IQ didn’t operate in a vacuum. Its business relied heavily on lead partners, advertising networks, and data-driven routing of consumers from websites and ads to call centers. The parallel settlement with MediaAlpha, a major player in lead distribution, underlines that the FTC is looking at the entire chainnot just the final seller.
If your business model depends on “hot leads” and aggressive outbound sales, the Assurance IQ case is basically a compliance horror story with a giant price tag attached.
Insurtech’s “move fast and break things” moment is over
A few years ago, the insurtech narrative was all about speed: scale quickly, buy leads, optimize funnels, and assume compliance can catch up later. This judgment sends the opposite message:
- Consumer protection comes first.
- Health coverage is too sensitive to be treated like generic e-commerce.
- “Growth at any cost” can end with regulators sending the bill.
When an acquisition that once looked like a $2.35 billion success story ends with a shutdown, huge write-downs, and a $100 million settlement, investors and executives in the space take notice.
Lessons for Consumers Shopping for Health Insurance Online
The most important takeaway for consumers is not “never shop online”it’s “shop smarter and verify everything.” Here are practical tips grounded in what the FTC flagged in the Assurance IQ case.
1. Treat “ACA-like” claims with skepticism
If a salesperson or website claims that a plan is “just like” an Affordable Care Act plan but much cheaper, that’s a red flag. ACA-compliant plans have to cover essential health benefits and follow rules on preexisting conditions. Short-term or limited-benefit plans typically do not.
Always ask directly:
- “Is this plan ACA-compliant?”
- “Does it cover preexisting conditions from day one?”
- “Is there an annual or lifetime cap on benefits?”
2. Demand the Summary of Benefits and Coverage (SBC)
Before you pay a premium, ask for written documentationespecially the Summary of Benefits and Coverage or comparable plan documents. That’s where exclusions, caps, and limitations live. If you’re only getting a verbal pitch or a vague brochure, hit pause.
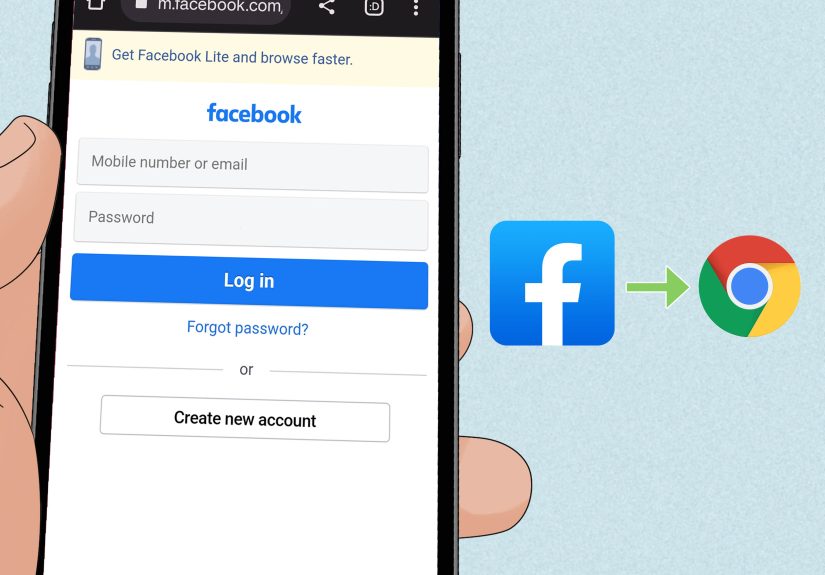
3. Be careful with online forms
Many consumers in the Assurance ecosystem reportedly entered their information into “quote” forms and then were hit with a wave of calls. If you give your phone number online, assume it might trigger aggressive outreach unless the site is a trusted marketplace or your insurer’s official portal.
Tips:
- Use official ACA marketplaces (like HealthCare.gov) or reputable carriers when possible.
- If you start getting repeated unsolicited calls, consider blocking numbers and reporting them.
- Don’t give payment information to a caller unless you’re sure which company they represent and you’ve verified the plan independently.
4. Document everything
If you’re promised specific coveragelike “yes, maternity is covered” or “no limit on doctor visits”write down the date, time, and name of the person you spoke to and keep any emails or texts. If things later go wrong, that documentation can be helpful in complaints or refund efforts.
Compliance Takeaways for Marketers and Insurtechs
For businesses, the Assurance IQ judgment is a checklist of what not to do. But it also points to a roadmap for compliant growth.
1. Align sales scripts with reality, not wishful thinking
If your product is a limited-benefit or short-term plan, your marketing and scripts must say so clearlyno implying “full coverage” where none exists. Claims about preexisting conditions, out-of-pocket costs, and networks should be backed by actual policy language, not sales enthusiasm.
2. Treat lead generation as a regulated activity
The days of “buy leads and look the other way” are over. The FTC’s broader $145 million action shows that regulators expect:
- Clear consumer consent for calls and data use,
- Transparency about who is calling and why,
- Controls over how partners collect, transfer, and use leads.
If your lead partner uses dark patterns, deceptive landing pages, or vague promises, you can’t simply claim ignorance; regulators increasingly treat downstream sellers as responsible for what happens upstream.
3. Telemarketing compliance is not optional
Telemarketing in health insurance sits at the intersection of the TSR, robocall rules, do-not-call regulations, and sometimes healthcare privacy obligations. That means you need:
- Documented consent for robocalls or prerecorded messages,
- Internal do-not-call policies and training,
- Systems to track and log outbound calls, and
- Routine audits of scripts and vendor performance.
Compliance might slow down your funnel by a few seconds, but it’s cheaper than a $100 million judgment.
Real-World Experiences and Scenarios Around the Assurance IQ Model
To understand why the FTC hit Assurance IQ so hard, it helps to picture what this looked like in real lifeboth at the consumer’s kitchen table and inside the call centers fueling the business.
A typical consumer journey: from “great deal” to big bills
Imagine a consumer in their late 50s, recently between jobs, staring at rising premiums on ACA marketplace plans. They see an ad promising “great coverage at a fraction of the cost,” click through a polished website, and enter contact details for a quote.
Within minutes, the phone rings. A friendly agent explains that there’s a “special plan” that works just like an ACA plan but costs a lot less each month. The call is fast-paced, peppered with reassurances:
- “Yes, it covers hospital stays.”
- “Yes, you can keep your doctor.”
- “Yes, preexisting conditions are fine.”
The consumer hears what they desperately want: full protection without full-price premiums. They give a payment method over the phone and feel relieved. Only months laterafter a surgery, a chronic condition flare, or an unexpected hospitalizationdo they discover that the plan pays out only a modest fixed amount per day or per visit, leaving them with thousands in uncovered costs.
This kind of experience, repeated at scale, is exactly what regulators pointed to when describing how consumers were misled into thinking they had comprehensive health insurance when they did not.
Inside the sales environment: pressure, scripts, and incentives
On the other side of the phone, you can imagine a call-center agent working off a script optimized for conversions. Performance metrics might include:
- Number of calls per hour,
- Conversion rate from inquiry to paid policy,
- Average premium size, and
- Upsells to additional products like discount cards or telemedicine bundles.
In that kind of environment, the line between “persuasive” and “deceptive” can erode quicklyespecially if training and oversight aren’t explicitly focused on compliance. Agents who stick to cautious, heavily qualified language might close fewer sales. Agents who gloss over limitations might become top performers, at least in the short term.
The FTC’s complaint suggests that, over time, the system rewarded the wrong behaviors: emphasizing the upside of plans without equal emphasis on the limitations. When that pattern shows up in call recordings, scripts, and consumer complaints, regulators see a structural problemnot just a few bad apples.
The wake-up call for companies: good intentions aren’t enough
Many insurtech and lead-generation companies genuinely believe they’re helping consumers find affordable options. But the Assurance IQ outcome shows that intent doesn’t outweigh impact. A company can say it wants to improve access and still end up on the wrong side of the law if its marketing leaves consumers confused or misled.
Executives watching this case unfold are drawing some painful but valuable lessons:
- “We thought our disclaimers were enough” is not a defense if the overall impression is misleading.
- “Everyone else markets this way” doesn’t work when regulators decide to reset industry norms.
- “We didn’t know our partners were doing that” is not persuasive when you profit from their leads.
As a result, many companies are revisiting their scripts, landing pages, and partner agreementstightening disclosures, slowing down calls to allow for explanation, and investing in real compliance programs. Nobody wants to be the next headline: “FTC secures nine-figure judgment against…”
For consumers, a small silver lining
While no settlement fully erases the stress of unexpected medical bills, the $100 million judgment and the broader $145 million package provide a measure of accountability. They signal that regulators are watching and that misleading health insurance marketing can have real consequences for the companies behind it.
The best “experience” going forward, for both consumers and businesses, is one where coverage is described clearly, expectations match reality, and nobody finds out what’s not covered only after a crisis.
Conclusion: A Landmark Case in Digital Health Insurance Marketing
The FTC’s $100 million judgment against Assurance IQ is more than a large number in a headline. It marks a turning point for how digital platforms sell health insurance, how lead-generation companies think about consent and transparency, and how regulators enforce consumer protection in an algorithm-driven marketplace.
For consumers, the message is clear: don’t take promises of “comprehensive coverage” at face value, especially when they come with rock-bottom prices and high-pressure sales. For businesses, the message is even clearer: build compliance into your growth strategyor regulators will build enforcement into your future.