Table of Contents >> Show >> Hide
- What Is Fundoplication?
- Uses: Why Fundoplication Is Done
- Types of Fundoplication (Nissen, Toupet, Dor)
- Who Is (and Isn’t) a Good Candidate?
- Pre-Surgery Testing: What You’ll Likely Need
- What Happens During the Procedure?
- Hospital Stay: How Long Will You Be There?
- Recovery: What to Expect Week by Week
- Diet After Fundoplication: The Big Rules (So You Don’t Hate Lunch)
- Benefits: What Fundoplication Can Improve
- Risks and Side Effects: The Not-So-Fun Part (But Important)
- Fundoplication vs Other Options
- FAQ
- Final Thoughts
- Experiences After Fundoplication (500+ Words): What People Commonly Notice
- The “Why does my shoulder hurt if my stomach got fixed?” moment
- Swallowing feels weirdlike food is “pausing”
- The “I miss burping” phase (and the bubble management era)
- Diet progression feels like leveling up in a video game
- Energy comes back… but not all at once
- The reflux relief can feel surprisingly quiet
If your stomach acid has been treating your esophagus like a slip-n-slide, you’ve probably heard the word
fundoplication. It sounds like a spell from a wizarding school, but it’s actually a well-established
anti-reflux surgery used to help control GERD (gastroesophageal reflux disease) and often repair a
hiatal hernia at the same time.
This guide breaks down what fundoplication is used for, how doctors decide who’s a good candidate, what the surgery
day usually looks like, and what recovery can feel likeright down to the “why do I feel like I swallowed a balloon?”
phase. (Spoiler: that part is common and usually temporary.)
What Is Fundoplication?
Fundoplication is a procedure that reinforces the valve between your esophagus and stomachyour
lower esophageal sphincter (LES). During surgery, the top part of the stomach (the
fundus) is wrapped around the lower end of the esophagus to strengthen the barrier that keeps acid and
stomach contents from flowing back up.
Most modern fundoplications are done using minimally invasive methods (usually laparoscopic, and
sometimes robotic). Small incisions, a camera, specialized instruments, and a surgeon who has done this more times
than you’ve reheated coffee.
Uses: Why Fundoplication Is Done
Fundoplication is most commonly performed as an anti-reflux surgery for people with GERD when symptoms
don’t improve enough with lifestyle changes and medicationsor when complications make surgery a better long-term
strategy.
Common reasons a doctor may recommend fundoplication
-
GERD that doesn’t respond well to medication, or symptoms that return quickly when medication is
stopped. -
Complications of reflux such as severe esophagitis (significant inflammation/erosion), strictures
(narrowing), or concern for ongoing injury. -
Large or symptomatic hiatal hernia contributing to reflux (surgery may repair the hernia and add the
wrap). - Regurgitation (food/acid coming back up) that remains a major quality-of-life problem even with PPIs.
-
A desire to avoid long-term reliance on acid-suppressing medication when surgery is appropriate and
GERD is objectively confirmed.
A quick “real-life” example
Imagine someone who’s on a high-dose PPI and still wakes up at night coughing, with sour fluid in the throat. An
endoscopy shows significant reflux injury, and testing confirms abnormal acid exposure. If anatomy (like a hiatal
hernia) and esophageal function line up, fundoplication can be consideredespecially when symptoms are disruptive and
persistent.
Types of Fundoplication (Nissen, Toupet, Dor)
“Fundoplication” isn’t one single wrapit’s a family of wraps. The main difference is how much the stomach is
wrapped around the esophagus.
-
Nissen fundoplication (360°): a complete wrap. Often used when esophageal motility is adequate and a
strong barrier is desired. -
Toupet fundoplication (270°): a partial posterior wrap. Sometimes chosen to reduce the risk of
swallowing trouble in certain patients. -
Dor fundoplication (180°): a partial anterior wrap, used in specific situations (sometimes alongside
other esophageal procedures).
Which one is “best” depends on your symptoms, anatomy, and results of pre-op testing. This is where shared
decision-making matters: your surgeon’s experience + your body’s data + your priorities.
Who Is (and Isn’t) a Good Candidate?
Fundoplication tends to work best when GERD is clearly documented and symptoms match the reflux
pattern. The goal is to avoid “wrong-problem, right-surgery,” which is about as fun as it sounds.
Doctors usually look for:
- Objective evidence of GERD (endoscopy findings and/or reflux monitoring)
- Symptoms that fit reflux (especially regurgitation and classic heartburn)
- Esophageal motility that can push food through the repaired area
- Anatomy that supports surgery (like a hiatal hernia that can be repaired)
Fundoplication may be less helpful if:
-
Symptoms are primarily functional (for example, heartburn-like symptoms without documented reflux) or driven by
non-reflux causes. -
There’s significant esophageal motility disorder that makes swallowing weakthis doesn’t always rule surgery out,
but it influences the type of wrap. -
Expectations are mismatched (example: hoping surgery will “cure” all chest discomfort when testing doesn’t confirm
reflux as the driver).
Pre-Surgery Testing: What You’ll Likely Need
Before fundoplication, many surgeons and GI specialists want to confirm two key things:
(1) reflux is truly happening and (2) your esophagus can move food effectively.
Common tests include
-
Upper endoscopy (EGD): checks for inflammation, erosions, Barrett’s changes, strictures, and other
issues. -
Ambulatory pH monitoring (often impedance-pH): measures acid exposure (and sometimes non-acid reflux)
over 24–96 hours. -
Esophageal manometry: measures the strength/coordination of esophageal muscle contractions and helps
rule out major motility disorders. -
Imaging (barium swallow / upper GI series): evaluates anatomy, swallowing mechanics, and hernia
features in many cases.
Tip: if someone schedules you for pH testing, plan for a day where you aren’t trying to impress anyone. It’s not
painful for most people, but it is… a vibe.
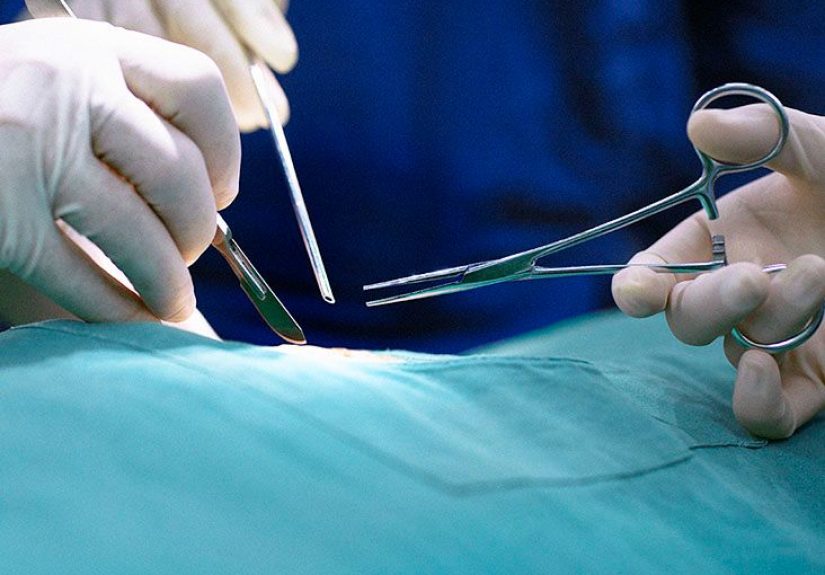
What Happens During the Procedure?
Fundoplication is performed under general anesthesia. In minimally invasive surgery, the surgeon makes
several small incisions, works with a camera and instruments, and builds the wrap around the lower esophagus.
If a hiatal hernia is present, it’s often repaired by repositioning the stomach and tightening the
diaphragm opening (the hiatus) so the stomach stays where it belongsdown in the abdomen, not moonlighting in the
chest.
How long does it take?
Timing varies depending on anatomy, hernia size, scar tissue, and surgical approach. Your surgical team can give the
best estimate for your specific case.
Hospital Stay: How Long Will You Be There?
Many people go home within 1–3 days after a laparoscopic fundoplication, depending on pain control,
nausea, ability to drink/eat per plan, and overall stability. Some people may go home sooner; others need longer,
especially after more complex hernia repairs.
Recovery: What to Expect Week by Week
Recovery isn’t usually dramatic, but it is specific. Your wrap area will be swollen at first, and your body needs time
to learn the new “traffic pattern” at the bottom of the esophagus.
The first 24–72 hours
- Soreness around incision sites and inside the abdomen is common.
-
Shoulder pain can happen from the gas used during laparoscopy irritating the diaphragm (annoying but
common). - You’ll be encouraged to walk early to reduce clot risk and help your gut wake up.
- You’ll start on a diet progression determined by your surgeon (often liquids first).
Week 1–2
- Low energy is normal. Your body spent the week doing construction workinternally.
-
Swallowing feels “tight” for some people due to swelling, especially with bigger bites or fast
eating. - Many patients follow a plan that starts with liquids or blenderized foods, then advances slowly.
Weeks 3–6
- You may transition to soft foods and gradually more texture.
-
Breads and dense meats can be tricky early on and are often delayed until later, depending on your
surgeon’s instructions. - Activity often increases gradually, but heavy lifting restrictions may applyespecially if a hernia repair was done.
2–3 months and beyond
-
Many people see big improvements in classic reflux and regurgitation, but some symptoms can take time
to settle (especially bloating and swallowing changes). -
Some people still need reflux medication occasionally, depending on their underlying condition and long-term
outcomes.
Diet After Fundoplication: The Big Rules (So You Don’t Hate Lunch)
Diet instructions vary by surgeon and by the complexity of surgery, but many plans share a theme:
start smooth, go slow, chew like it’s your job.
Common diet principles
- Small, frequent meals instead of big plates.
- Chew thoroughly and eat slowlyrushing is the enemy of a happy wrap.
- Avoid carbonated beverages early on (bubbles + new wrap = discomfort for many).
- Be cautious with sticky or dense foods early (bread, tough meats), depending on your stage.
- Stay hydrated, but avoid “chugging.” Think sipping, not marathon water gulps.
What a sample progression can look like (varies by provider)
- Stage 1: clear liquids
- Stage 2: full liquids / blenderized foods
- Stage 3: soft foods
- Stage 4: gradual return to regular texture as tolerated
Always follow your surgeon’s planespecially if your case involved a larger hiatal hernia repair or additional steps.
Benefits: What Fundoplication Can Improve
The primary goal is to reduce reflux by strengthening the LES barrier. Many patients experience:
- Less heartburn and regurgitation
- Improved sleep due to fewer nighttime reflux episodes
- Reduced dependence on reflux medications (in many, not all)
- Better control of reflux symptoms linked to a hiatal hernia after repair
Risks and Side Effects: The Not-So-Fun Part (But Important)
Every surgery has risks. With fundoplication, most concerns fall into two categories:
general surgical risks and wrap-specific side effects.
General surgery risks (examples)
- Bleeding, infection
- Reactions to anesthesia
- Blood clots (risk reduced by early walking and prevention strategies)
Wrap-specific side effects people often ask about
-
Temporary difficulty swallowing (dysphagia): common early due to swelling; persistent symptoms should
be evaluated. -
Gas-bloat symptoms: bloating, increased gas, discomfort after eatingoften improves with time and
diet adjustments. -
Difficulty burping or vomiting: a tighter barrier can make “letting air out” harder at first (and in
some cases longer-term). - Diarrhea or bowel changes: can occur in some patients after anti-reflux surgery.
-
Recurrent reflux or wrap failure: symptoms can recur if anatomy changes over time (for example,
hernia recurrence) or if the wrap loosens/slips.
When to call your surgeon or seek urgent care
- Fever, worsening redness/drainage from incisions
- Inability to keep liquids down, severe dehydration signs
- Worsening chest pain, severe shortness of breath
- Severe or progressive swallowing difficulty
Fundoplication vs Other Options
Surgery is one tool in the GERD toolbox. Depending on your situation, your team may discuss:
- Medication optimization (PPI timing, dose, adding nighttime strategies, lifestyle).
-
Endoscopic anti-reflux approaches for select patients (for example, transoral incisionless
fundoplication in appropriate candidates). - Other surgical options in specific scenarios, especially when anatomy or hernia type changes the plan.
The “right” option depends on confirming reflux, understanding anatomy, and matching the approach to the problem.
FAQ
Will fundoplication cure GERD forever?
Many people get long-term reliefespecially from regurgitationbut outcomes vary. Some patients eventually need
reflux medication again, and a smaller group may need further evaluation for recurrent symptoms.
Is fundoplication painful?
Expect soreness and fatigue early on. Pain is typically manageable with a plan from your care team. Shoulder pain from
laparoscopic gas is common and usually improves as the gas is absorbed.
How soon can I return to normal activities?
Walking is encouraged early. More strenuous activity and heavy lifting are usually restricted for a period of time,
especially after hernia repair. Your surgeon will give personalized guidance.
Can I still burp after a fundoplication?
Some people can burp, some can’t (at least at first). The ability often improves as swelling goes down, but it varies
depending on wrap type and individual anatomy.
Final Thoughts
Fundoplication is a time-tested option for people with documented refluxespecially when medications aren’t enough,
regurgitation is a major issue, or a hiatal hernia is part of the story. The best outcomes usually come from good
pre-op testing, careful patient selection, and a recovery plan that respects two truths:
your wrap needs time, and your fork needs patience.
If you’re considering surgery, talk with a gastroenterologist and an experienced surgeon about your test results,
your specific symptoms, and what success looks like for you.
Experiences After Fundoplication (500+ Words): What People Commonly Notice
The internet is full of dramatic storiessome inspiring, some terrifying, and some written at 2 a.m. while someone is
eating pudding with the intensity of an Olympic sport. To keep things grounded, here are common experiences patients
often report after fundoplication, framed in a realistic “what it can feel like” timeline. (This isn’t a promise or a
predictionjust a practical preview of what many people describe.)
The “Why does my shoulder hurt if my stomach got fixed?” moment
Early after laparoscopic surgery, some people are surprised by shoulder or upper chest discomfort. This can happen
because the gas used during surgery irritates the diaphragm, which shares nerve pathways that “refer” sensation to the
shoulder. Translation: your body is sending the complaint letter to the wrong department. Walking, gentle movement,
and time often help.
Swallowing feels weirdlike food is “pausing”
A very common experience in the first couple of weeks is a tight or delayed feeling when swallowing, especially with
thicker foods. People often describe it as food “hanging up” briefly before passing. This is frequently related to
swelling around the wrap area. Many patients learn quickly that tiny bites, slow eating, and thorough chewing turn a
stressful meal into a manageable one. Some even develop a new superpower: the ability to detect an over-confident bite
before it happens.
The “I miss burping” phase (and the bubble management era)
Because the new barrier is stronger, some patients feel more bloated or gassy early onespecially if they drink
carbonated beverages, use straws, chew gum, or eat too fast (all of which can increase swallowed air). People often
experiment with “bubble control” strategies: skipping soda, choosing warm tea over fizzy drinks, eating smaller meals,
and avoiding gas-producing foods for a bit. Many report that bloating improves over time, but patience is the name of
the game here.
Diet progression feels like leveling up in a video game
A lot of people describe the post-op diet as a structured series of levels: clear liquids → full liquids →
blenderized/soft foods → gradual return to normal texture. The good news: it’s straightforward. The hard part: it can
feel repetitive. Patients often say the “win” is finding a rotation of high-protein soft foods that don’t taste like
punishmentthink smooth soups, yogurt (if tolerated), protein shakes, scrambled eggs, mashed beans, and soft-cooked
grains. The key habit that shows up again and again is eating slowly and stopping before fullness turns into pressure.
Energy comes back… but not all at once
People frequently report lower stamina for a whileeven if the incisions look small. That’s because the healing work is
happening internally. It’s common to feel okay one day and then feel wiped out the next after doing “normal stuff.”
Many patients find success by building activity gradually: short walks multiple times per day, then longer walks, then
light errands, then a careful return to more demanding routines when cleared.
The reflux relief can feel surprisingly quiet
Some of the most positive experiences aren’t dramaticthey’re subtle. People notice they can lie down without
immediate burning. Nighttime cough improves. Regurgitation fades. And for many, the biggest emotional shift is simply
not planning life around reflux: no more sleeping propped up like a museum exhibit, no more “acid math” after every
meal, no more wondering if a tomato looked at them wrong.
Bottom line: many recoveries include a mix of relief, adjustment, and a learning curve with eating. If symptoms feel
severe, persistent, or progressively worseespecially trouble swallowing or dehydrationpatients often do best when
they contact their surgeon early rather than trying to “tough it out.”