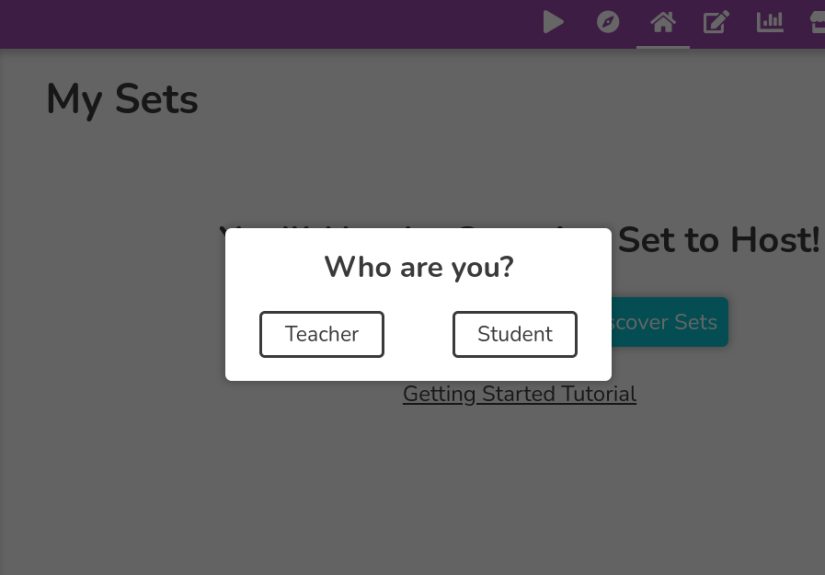
Table of Contents >> Show >> Hide
- The “24-hour rule” and the “6-week rule”
- What are hives, exactly?
- How long can hives last? Typical healing timelines
- Why hives can “move around” and still be the same outbreak
- What makes hives last longer?
- Common triggers (and how fast they can act)
- Treatment that helps (and what usually doesn’t)
- When hives are an emergency
- When to see a clinician (even if it’s not an emergency)
- How clinicians figure out what’s going on
- Outlook: how long until you’re “back to normal”?
- Real-world experiences: what hives timelines look like in everyday life (about )
- Conclusion
Hives have a special talent: they can show up out of nowhere, itch like they’re auditioning for an award, and then
disappear as if nothing happenedonly to pop up somewhere else five minutes later. If you’re staring at your skin
thinking, “How long is this going to last?” you’re not being dramatic. You’re being practical.
The good news: most cases are short-lived, and individual hives are usually temporary. The tricky part: the
episode can last longer than any single welt, because new ones can keep arriving like uninvited guests who
refuse to read the room.
The “24-hour rule” and the “6-week rule”
Two timelines explain most hive situations:
-
The 24-hour rule: A single hive (one raised, itchy bump) typically fades within 24 hours, often
much soonereven if a new one appears nearby. -
The 6-week rule: If hives keep coming back for 6 weeks or longer, that’s
considered chronic urticaria (chronic hives).
So if you feel like your hives are “lasting forever,” it may be that individual welts are cycling quickly while the
overall outbreak is still active.
What are hives, exactly?
Hives (also called urticaria) are raised, itchy welts caused by chemicalsespecially
histaminereleased in the skin. They can be tiny pinpricks, big patches, or ring-shaped welts that
look like your skin is playing abstract art.
Sometimes hives come with angioedema, which is deeper swelling under the skin (often around the lips,
eyelids, hands, feet, or genitals). Angioedema can feel tight, puffy, or even achy rather than just itchy.
How long can hives last? Typical healing timelines
1) One hive: minutes to (usually) under 24 hours
Most individual hives appear quickly and fade within 24 hours. They may shift locations, change shapes, or merge into
larger areas and then break apart again. That “moving target” behavior is common.
2) Acute hives: a few hours to a few weeks (and always under 6 weeks)
Acute urticaria is the medical term for hives that last less than 6 weeks. Many acute episodes clear
in a few days. Others come and go for a couple of weeksespecially when a trigger (like a viral illness) is still in
the background.
3) Chronic hives: 6 weeks or longer (often months, sometimes years)
Chronic urticaria means hives that recur for 6 weeks or more. This doesn’t mean you’ll have welts
24/7 forever. It often comes in wavescalm stretches and flare-ups. For many people, chronic hives eventually improve
over time, but the timeline can be unpredictable.
4) Physical (inducible) hives: often short, but repeatable
Some people get hives from physical triggers like heat, cold, pressure, vibration, sunlight, or exercise. In these
cases, welts may show up within minutes and fade within hoursthen return the next time the trigger happens.
Why hives can “move around” and still be the same outbreak
Hives are famous for shape-shifting. One spot calms down, another lights up. That’s because the reaction is happening
across the skin’s surface, and histamine release can flare in different places at different times. It can look like
the rash is spreading, when it’s actually a series of short-lived welts rotating through your body’s “itchy
spotlight.”
What makes hives last longer?
Hives aren’t one-size-fits-all. These factors often stretch out an outbreak:
-
The trigger is still present: ongoing infection, continued exposure to an allergen, or a medication
your body doesn’t like. -
Heat and sweating: hot showers, tight clothing, workouts, and warm rooms can amplify itching and
welts. -
Scratching: it can create more inflammation and can trigger “scratch hives” (dermatographism) in
some people. -
Stress and poor sleep: not “all in your head,” but stress hormones and sleep loss can make symptoms
feel louder and harder to settle. -
NSAIDs and alcohol (for some people): medications like ibuprofen or naproxen, and alcohol, can
worsen hives in certain individuals.
Common triggers (and how fast they can act)
Allergies: foods, medications, insect stings
True allergic hives can appear quicklysometimes within minutes to a couple hours after exposure. Common culprits
include certain foods, antibiotics, and insect stings. Not every hive outbreak is an allergy, but if the timing is
consistent (same food, same reaction), it’s worth medical attention.
Viral infections (a very common “mystery trigger”)
Colds and other viral illnesses are frequent causes of acute hives, especially in kids and teens. Sometimes hives show
up near the end of the illnesslike your immune system’s dramatic encore.
Contact and environment
New detergents, fragranced lotions, plants, latex, pet dander, and even pressure from straps or waistbands can be
involved. Contact triggers can cause local hives where the skin touched the irritantor contribute to a more general
flare.
Physical triggers
Cold urticaria (cold exposure), cholinergic urticaria (heat/exercise), pressure urticaria (tight clothing or carrying
bags), and solar urticaria (sunlight) can create repeatable patternsuseful clues for diagnosis.
Treatment that helps (and what usually doesn’t)
First-line: non-drowsy antihistamines
For most people, the first and most effective tool is a second-generation H1 antihistamineoften
called “non-drowsy” (though some people still feel sleepy). Examples include cetirizine, loratadine, levocetirizine,
and fexofenadine.
Practical tip: if hives are recurring, clinicians often recommend taking an antihistamine on a schedule (rather than
only “when it gets bad”), because consistent histamine-blocking can prevent the next wave from building momentum.
Always follow label directions unless a clinician specifically advises otherwise.
Short-term extras (when symptoms are intense)
Depending on the situation, a clinician may recommend additional options such as:
-
Short courses of oral steroids for severe acute flares (not a long-term solution, and not right for
everyone). -
Trigger management (stopping a suspected medication under medical guidance, treating an infection,
avoiding a confirmed food trigger). - Soothing measures (see below) to reduce itch and skin irritation.
For chronic hives that don’t respond well to antihistamines
Chronic hives can require a step-up plan with a specialist (allergist/immunologist or dermatologist). Common
next-level strategies include:
-
Antihistamine “up-dosing” under medical supervision (some guidelines support higher doses for
resistant cases). -
Biologic therapy such as omalizumab (an FDA-approved option for chronic
spontaneous urticaria in appropriate patients). - Other prescription approaches for difficult cases, chosen based on your history and risk factors.
Home care that actually makes the day better
- Cool compresses for 10–15 minutes when itching spikes.
- Lukewarm showers (hot water can make hives angrier).
- Loose, breathable clothing to reduce friction and heat.
- Fragrance-free moisturizer to calm irritated skin.
- Colloidal oatmeal baths or gentle anti-itch lotions for symptom relief.
- Keep nails short to reduce skin damage if you scratch in your sleep.
What usually doesn’t help much: trying to “detox,” aggressively scrubbing the rash, or switching skincare products
repeatedly (which can add irritation). Hives are an immune/chemical reaction, not dirt you can power-wash off.
When hives are an emergency
Call emergency services right away if hives are accompanied by signs of a severe allergic reaction, such as:
trouble breathing, wheezing, throat tightness, swelling of the lips/tongue/throat, fainting, severe dizziness, or
widespread symptoms that escalate fast. If someone has prescribed epinephrine for severe allergies, use it as directed
and get emergency care immediately.
When to see a clinician (even if it’s not an emergency)
Consider medical evaluation if any of these are true:
- Hives recur or persist for 6 weeks or more.
- You’re getting hives frequently, or they disrupt sleep, school, or work.
- You have repeated angioedema (deep swelling), especially around the face.
-
Welts are painful rather than itchy, last in the same spot longer than 24 hours,
or leave bruising/discoloration (this can suggest a different condition that needs evaluation). - You started a new medication or supplement shortly before the outbreak.
- You have fever, joint pain, or other systemic symptoms along with the rash.
How clinicians figure out what’s going on
For acute hives, diagnosis is often based on your story: what you ate, what you touched, medications taken, recent
illness, insect stings, and the timing. For chronic hives, testing is sometimes limited and targeted. Many chronic
cases are “spontaneous,” meaning no clear trigger is found even after a careful workupand that can still be treated
effectively.
A simple tracking method that helps (without turning life into a spreadsheet)
- Take photos when hives appear (helpful for appointments).
- Note the time they started and how long a single welt lasts.
- List obvious exposures in the prior 6–12 hours (foods, meds, exercise, heat/cold, new products).
- Record what helped (antihistamine, cool compress, avoiding heat) and how quickly it worked.
Outlook: how long until you’re “back to normal”?
If you have acute hives, the most common outcome is that they settle within days to a few weeks, especially once the
trigger fades or is removed. If you have chronic hives, it may take longer to find a plan that keeps flare-ups under
controlbut many people do get good relief with a stepwise treatment approach.
The goal isn’t to “tough it out.” The goal is to reduce itch, prevent flares, protect sleep, and make sure nothing
more serious (like anaphylaxis or a non-hive rash that behaves differently) is being missed.
Real-world experiences: what hives timelines look like in everyday life (about )
The “new laundry detergent” surprise (2–4 days)
A common story: someone switches detergent to a “fresh mountain breeze” brand that smells like confidence and
questionable decisions. Within a day, itchy welts show up along the waistband, underarms, or anywhere clothing rubs.
Individual hives fade in hours, but new ones appear after each outfit change. Once the detergent is removed (rewash
clothes, switch back, go fragrance-free), the outbreak often calms down over a few daysespecially with a non-drowsy
antihistamine and cooler showers. The lesson people take away is simple: the skin sometimes votes “no” on scented
products, and it votes loudly.
The “viral bug encore” (1–3 weeks)
Another frequent pattern happens after a cold or stomach virus. The fever is gone, energy is returning, and thenbam:
hives. Because they come and go, it feels like the rash is “chasing” you around your body. People often notice that
heat, stress, and late nights make it worse, while consistent antihistamines and good sleep make it quieter. The
frustrating part is timing: you feel “almost better,” but your immune system is still cleaning up, and the skin gets
caught in the crossfire. In many cases, the hives fade as the immune system fully settles.
The “workout reaction that wasn’t poison ivy” (minutes to hours, repeating)
Some people get hives primarily with exercise, hot weather, or strong emotionssmall, itchy bumps that flare during a
workout and ease afterward. The first time it happens, it can be scary (“Am I allergic to the gym?”), but patterns
help: it shows up with sweating, peaks fast, and fades within hours. People who manage it well often focus on cooling
strategies: lighter clothing, cooler environments, pacing, and sometimes pre-planned medical guidance if symptoms are
predictable. The key “aha” moment is realizing the timeline is short, but the trigger is repeatableso prevention can
be powerful.
The “NSAID plot twist” (days to weeks)
Another real-world experience: someone takes an NSAID (like ibuprofen) for a headache or sports soreness and notices
hives later that day or the next. It doesn’t happen to everyone, but for some, NSAIDs can worsen hives or make them
easier to trigger. The confusing part is that the person might have taken the same medication before with no problem.
Once they connect the dots, avoiding that trigger (with clinician guidance for safe alternatives) can shorten future
outbreaks dramatically. Many people come away from this one with a healthy respect for timing and a renewed habit of
checking what they took before symptoms started.
The “chronic mystery that finally got manageable” (months)
Chronic hives are often the most emotionally exhausting, not because every day is the worst day, but because the
unpredictability wears people down. Many describe a cycle: a good week, then a flare during exams, a weather swing, or
after poor sleepfollowed by a scramble of trial-and-error. People who eventually feel better often mention two
turning points: (1) getting a clear diagnosis that it’s chronic urticaria (not contagious, not “dirty,” not a moral
failure), and (2) finding a structured, stepwise plan with a specialist. Even when the cause stays unclear, the
symptom control can become clearand that’s a big quality-of-life win.
Conclusion
If you’re trying to predict how long hives can last, remember this: most individual welts fade within 24 hours, but
the overall episode can last days to weeksand if it keeps returning for 6 weeks or more, it’s considered chronic.
The right treatment plan (often starting with non-drowsy antihistamines), smart trigger management, and a few
itch-reducing habits can make the timeline feel shorter and the symptoms far more tolerable.
And if hives come with breathing trouble, throat swelling, or severe dizziness, don’t “wait it out.” That’s the moment
to treat it as urgent.