Table of Contents >> Show >> Hide
Getting diagnosed with celiac disease can feel like someone just deleted half your pantry with one click. Bread? Gone. Sunday donuts? Gone. Grandma’s secret lasagna recipe? Also gone… or at least it seems that way at first.
The good news: life with celiac disease is absolutely manageablefor both kids and adultsonce you understand what’s going on in your body and how to work with (not against) a strict gluten-free lifestyle. People of all ages with celiac can have healthy intestines, strong bones, and a full social life; the key is consistent, lifelong gluten avoidance and smart day-to-day habits.
This guide walks through what celiac disease actually is, how to build a safe gluten-free routine, special challenges for children and adults, and real-world tips to help your family thrive rather than just “get by.”
Quick reminder: This article is for education, not diagnosis or medical advice. Always talk with a healthcare professional or dietitian who knows celiac disease well before making major changes.
What Is Celiac Disease, Really?
Celiac disease is an autoimmune disorder. When someone with celiac eats glutena protein found in wheat, barley, and ryethe immune system overreacts and attacks the lining of the small intestine. Over time this damage interferes with nutrient absorption and can lead to problems such as anemia, poor growth in kids, osteoporosis, and increased risk of some cancers if it’s left untreated.
Important detail: celiac is not the same as a wheat allergy or non-celiac gluten sensitivity. It is a lifelong condition; you don’t “grow out of it,” and there’s currently no pill, shot, or surgery that cures it. The only proven treatment is a strict gluten-free diet for life.
Symptoms Can Look Different in Kids vs. Adults
Children may show classic digestive symptoms like chronic diarrhea, constipation, bloating, poor growth, short stature, or irritability. Adults might have digestive issuesor none at alland instead notice fatigue, anemia, bone pain, brain fog, migraines, infertility, or depression.
That wide range of symptoms is part of why diagnosis can be delayed, especially in adults. Once the diagnosis is confirmed, though, treatment is the same at every age: a carefully managed gluten-free lifestyle.
Gluten-Free Basics for All Ages
Think of the gluten-free diet as a lifelong project: phase one is learning the rules, phase two is living them in real life (a bit messier, a lot more trial and error), and phase three is feeling like it’s just your “normal.”
Meet BROWS: The Gluten-Containing Grains
A handy way to remember the main gluten culprits is the acronym BROWS:
- Barley
- Rye
- Oats* (we’ll explain in a second)
- Wheat
- Spelt (a type of wheat)
*Oats themselves are naturally gluten-free, but they’re often contaminated with wheat or barley during growing or processing. In the United States, oats used in gluten-free products must meet the same FDA gluten-free standard as any other ingredient, meaning the finished product must contain less than 20 parts per million (ppm) of gluten. To be safe, most people with celiac should only use oats that are clearly labeled “gluten-free.”
Build Meals Around Naturally Gluten-Free Foods
While you’re learning to decode food labels, it’s less stressful to focus on simple, naturally gluten-free foods that don’t need detective work:
- Fruits and vegetables
- Plain meats, poultry, fish, eggs, and most legumes
- Dairy like milk, yogurt, and cheese (watch flavored varieties for additives)
- Gluten-free grains and starches such as rice, quinoa, corn, potatoes, and certified gluten-free oats
- Nuts, seeds, and healthy oils
Then layer in packaged gluten-free products as you get more comfortable reading ingredient lists and understanding “gluten-free” labeling rules.
Label Reading and the U.S. Gluten-Free Rule
In the U.S., the FDA allows a “gluten-free” label only if the food contains less than 20 ppm gluten. That standard applies whether the food is naturally gluten-free or has gluten removed. For people with celiac disease, this threshold is considered low enough for most to safely consume.
Practical tips:
- Learn the obvious gluten words (wheat, barley, rye, malt, graham, semolina, durum, spelt, triticale).
- Be cautious with “may contain” or “processed in a facility with wheat” statementstalk to your dietitian about your comfort level.
- Be especially careful with soups, sauces, gravies, soy sauce, veggie burgers, meat substitutes, and seasonings, which often hide gluten.
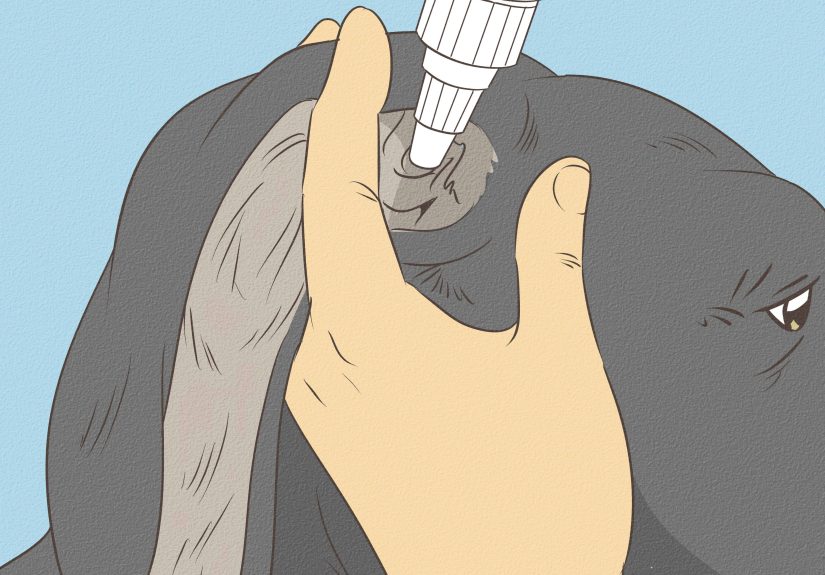
Preventing Cross-Contact at Home
Cross-contact happens when gluten-free food touches gluten-containing food, crumbs, or surfaces. Even small amounts can damage the intestine, even if you don’t feel symptoms.
Consider:
- Having a separate gluten-free toaster, cutting boards, and colanders.
- Keeping butter, jams, and spreads “double-dip-free” or having gluten-free-only versions.
- Training the whole household about clean counters and utensils.
Helping Kids Live Well With Celiac Disease
For children, celiac disease is not just about food; it affects school, social life, and self-image. Many kids feel different or left out at first. The goal is to normalize their gluten-free lifestyle while still keeping them safe and included.
Explaining Celiac to a Child
Use age-appropriate language. For younger kids, something like, “Your tummy gets hurt by a protein called gluten. So your job is to be a gluten detective and only eat foods that are safe for your super-hero tummy.” For teens, you can talk more frankly about autoimmune disease, long-term health, and the importance of sticking to the diet even when no one is watching.
Focus on what they can eat. Involve them in choosing safe snacks, cooking meals, and reading labels so they feel empowered, not punished.
School, 504 Plans, and Safety
School is where kids spend a huge chunk of their day, and unfortunately, it’s also where surprise cupcakes, pizza parties, and pasta projects tend to pop up. Children with celiac disease in the U.S. may qualify for a 504 plan, a legal accommodation plan under the Americans with Disabilities Act that outlines what the school must do to keep them safe and included.
Common 504 accommodations include:
- Providing gluten-free meals or allowing the child to bring safe food.
- Ensuring classroom projects and rewards (like stickers or candy) are gluten-free.
- Training staff to recognize symptoms of gluten exposure and to avoid cross-contact.
- Allowing the child to eat snacks in class when other kids are having gluten-containing treats.
Even if you don’t pursue a formal 504 plan, communicating clearly with teachers, the school nurse, and cafeteria staff is essential.
Birthdays, Playdates, and Holidays
Social events are where a gluten-free lifestyle really gets tested. A few kid-approved strategies:
- Always have a backup treat. Keep a stash of cupcakes, cookies, or snacks in the school freezer or your bag so your child has something fun when surprise treats appear.
- Talk to hosts ahead of time. Offer to bring a gluten-free pizza or dessert so your child can eat alongside everyone else.
- Practice self-advocacy scripts. Teach your child to say, “I have celiac disease, so I need to check if this is gluten-free before I eat it.”
Supporting Growth and Nutrition
Once a child goes strictly gluten-free, their intestines can heal, and their growth and nutrient absorption usually improve significantly. Many kids report better energy, fewer tummy aches, and improved mood after some months on a gluten-free diet.
But it’s easy to slide into a “gluten-free junk food” diet. Work with a pediatric dietitian to make sure your child’s meals include fiber, iron, calcium, vitamin D, and other key nutrients, not just gluten-free crackers and cookies.
Adult Life With Celiac Disease
Adults often face a different set of challenges: navigating work lunches, dating, travel, and long-term health concerns like bone density and fertility.
Eating Out Without Panic
Restaurant dining can be done safely, but it takes some strategy:
- Look for restaurants with dedicated gluten-free menus or celiac-aware policies.
- Call ahead and ask specific questions about cross-contact (shared fryers, grills, or prep surfaces).
- At the table, clearly say “I have celiac disease and need my food to be gluten-free with no cross-contact.”
- Simple dishesgrilled meats, salads without croutons, plain baked potatoesare often safer than heavily sauced or fried items.
Work, Travel, and Social Life
Office pizza Fridays, conference buffets, and airplane snacks can be land mines. Try:
- Keeping gluten-free bars, nuts, and jerky in your desk, bag, or car.
- Bringing your own food to meetings or potlucks and serving yourself first to avoid cross-contact.
- On trips, booking accommodations with a small kitchen, scouting grocery stores ahead of time, and packing a mini travel kit with a cutting board, sponge, and a few utensils.
Dating with celiac disease can be awkward initially (“Nice to meet you, by the way your kitchen crumbs can injure my intestines”), but it quickly becomes normal with the right partner. Consider choosing first-date spots where drinks or naturally gluten-free meals are easy, like coffee shops or restaurants with clear allergen labeling.
Long-Term Health: Beyond the Gut
For adults, untreated or poorly managed celiac disease increases the risk of complications like osteoporosis, anemia, infertility, and some cancers, and it’s strongly linked with lower quality of life and higher rates of depression and anxiety.
Key long-term steps include:
- Regular follow-up with your healthcare team to monitor antibody levels, nutrient status, and bone health.
- Bone density scans as recommended, especially if diagnosis was delayed or you have other risk factors.
- Mental health support if you’re struggling with anxiety, social isolation, or low mood.
Emotional Health for Kids and Adults
Celiac disease doesn’t just change your diet; it changes how you interact with people, how you travel, how you celebrate, and sometimes how you see yourself. Studies show that both children and adults with celiac disease often report lower quality of life and higher levels of anxiety or depression, especially when diagnosis is delayed or when social support is weak.
Some emotional survival tips:
- Validate that it’s hard. You’re allowed to grieve the loss of your favorite foods and the ease of eating anything, anywhere.
- Connect with others. Local celiac groups, online communities, and camps for kids with celiac can make a huge difference.
- Use humor when you can. You can’t eat the office donutsbut you can joke that at least you’ve finally found a diet you’ll actually stick to.
- Seek professional help. If anxiety about food or social situations is taking over, a therapist familiar with chronic illness can help you rebuild confidence.
Building a Celiac “Support Toolkit”
Think of managing celiac disease as building a toolkit. Over time you’ll collect:
- A list of go-to safe brands and products.
- Favorite gluten-free recipes your family actually loves.
- Backup snacks in your bag, car, work drawer, and kid’s backpack.
- Standard scripts for explaining your needs at restaurants, school, or social events.
- A healthcare team: gastroenterologist, dietitian, and, if needed, mental health professional.
Many people also create a “gluten sick day box” with electrolyte drinks, safe crackers, ginger tea, or other comfort items to use if they’re accidentally exposed to gluten. It doesn’t undo the exposure, but it can make you feel more cared for while your body recovers.
Real-Life Experiences: What Living With Celiac Really Feels Like
Guidelines and studies are important, but day-to-day life with celiac disease happens in real kitchens, classrooms, and coffee shops. To make this practical, let’s walk through what the gluten-free lifestyle can look like across different ages and situations.
Morning in a celiac household might start with everyone heading to the kitchen, but there’s a clear system. The gluten-free toaster is on one side of the counter, clearly labeled. The bread is stored in its own bin. A parent double-checks lunchboxes: the younger child has a thermos of gluten-free pasta and veggies, a container of cut fruit, and a labeled gluten-free cookie for the class birthday party. The older sibling, a teen, packs a burrito-style rice bowl and a protein bar they personally vetted by reading the ingredient list three times.
At school, the elementary-aged child walks into class and spots a tray of cupcakes. Five years ago this might have triggered panic or tears; now, there’s already a gluten-free cupcake waiting in the classroom freezer. The teacher pulls it out, the child sits with their classmates, and the moment feels like any other celebration instead of an episode of exclusion.
Meanwhile, the teenager heads to a friend’s house after school. Before going, they text: “Hey, I have celiac, so I can’t eat gluten. Can we order from that place with the gluten-free pizzas?” That one messageshort, clear, and confidentcomes from years of practicing how to advocate for themselves. They know exactly what questions to ask the restaurant about separate prep space and whether the crust is cooked on a clean pan.
For an adult newly diagnosed in their thirties, the early months can feel like starting over. That favorite sandwich shop? Off the list. Weekly beer with coworkers? Suddenly complicated. But after some trial and error, patterns emerge: a couple of reliable restaurants, a mental list of safe dishes, and coworkers who now ask, “Is there something gluten-free on the menu for you?” when planning team lunches.
Travel days are where preparation really shines. A parent of a child with celiac disease might pack an entire carry-on of shelf-stable snacks, instant oatmeal cups made with certified gluten-free oats, and a small cutting board and knife. They’ve already contacted the airline about bringing medical food onboard and mapped out grocery stores near the hotel. Instead of spending the trip hungry, the family spends it exploringbecause the food logistics were handled ahead of time.
There are also the “oops” moments. Almost everyone living with celiac disease experiences accidental exposure at some point: a sauce that wasn’t actually gluten-free, a fryer that shared space with breaded foods, a well-meaning relative who didn’t realize that “just a little bit” still counts. Having a planwho to call, what comfort foods or drinks help, and how to restturns a scary situation into a frustrating but manageable setback instead of a full-blown crisis.
Emotionally, many people describe a shift over time. Initially, the diagnosis may feel like a restriction-heavy sentence: “I can’t eat this, I can’t go there, I can’t just be spontaneous.” But as symptoms improve and energy returns, the narrative often changes. Some adults realize their “normal” exhaustion or bloating was never normal at all. Kids who were small for their age suddenly start growing. Parents see a child’s mood brighten after months of reliable gluten-free eating.
There’s also a sense of community that grows along the way. Parents trade lunchbox ideas in online groups. Adults share restaurant reviews and product recommendations. Entire threads are devoted to debating the best gluten-free brownies on the market. And while no one asks for celiac disease, many people say that it nudges them toward more intentional eating, stronger self-advocacy skills, and a deeper awareness of how food affects their bodies.
In other words, living with celiac disease is not a one-time decision; it’s a daily practice. Some days it will feel easy, some days it will feel unfair, but with knowledge, planning, and support, it can absolutely become just one part of a full, satisfying lifenot the whole story.
The Bottom Line
Living with celiac diseaseat any agemeans becoming a lifelong expert in your own health. Kids need clear communication, safe school plans, and inclusive social experiences. Adults need strategies for eating out, traveling, and protecting long-term health. Everyone needs good nutrition, emotional support, and a plan to handle the occasional curveball.
Strict gluten-free eating is non-negotiable for celiac disease, but so are joy, connection, and good food. With time, your gluten-free life can feel less like a restriction and more like a customized lifestyle that keeps you and your family feeling strong, energized, and fully present.