Table of Contents >> Show >> Hide
- The Urgent Care Wake-Up Call (And Why It Got Everyone’s Attention)
- What Exactly Is the “Triangle of Death” (AKA the Danger Triangle)?
- Why Popping a Pimple Can Backfire (Even Outside the Triangle)
- So What Can Go Wrong in the Danger Triangle?
- How Common Is This, Really?
- Red Flags: When a Pimple Stops Being “Just a Pimple”
- What Urgent Care or the ER Might Do
- Safer Alternatives: How to Treat a Deep, Painful Pimple Without the Drama
- Why the Triangle of Death Warning Is Worth Respecting
- Conclusion: Keep the Popcorn, Skip the Pimple-Popping
- Real-Life Experiences: of “I Wish I’d Known That”
There are two kinds of people in this world: the ones who can leave a pimple alone, and the ones who treat their bathroom mirror like an operating room.
If you’re in Group Two, you’re not alone—and you’re also exactly who doctors are talking to when they beg: please stop popping,
especially in the so-called “Triangle of Death” on your face.
That name sounds like it belongs in an action movie trailer. Unfortunately, it’s real anatomy, and while serious complications are rare, the consequences
can be severe enough that physicians keep warning people not to mess with pimples in that zone.
The Urgent Care Wake-Up Call (And Why It Got Everyone’s Attention)
Recently, a mom shared a scary (and very relatable) story: she popped a stubborn pimple near her nose—right inside the danger triangle—and
woke up the next day with intense facial pain, concerning facial symptoms, and vision issues that sent her to urgent care. She was treated promptly
with medications (including antibiotics), and thankfully improved quickly.
Stories like this travel fast because they hit a nerve: acne is common, stress is real, and the urge to “just get it out” is basically
hardwired into the human brain. But the medical takeaway is simple: popping a pimple can turn a small skin problem into a bigger infection,
and the mid-face has a unique pathway that makes doctors extra cautious.
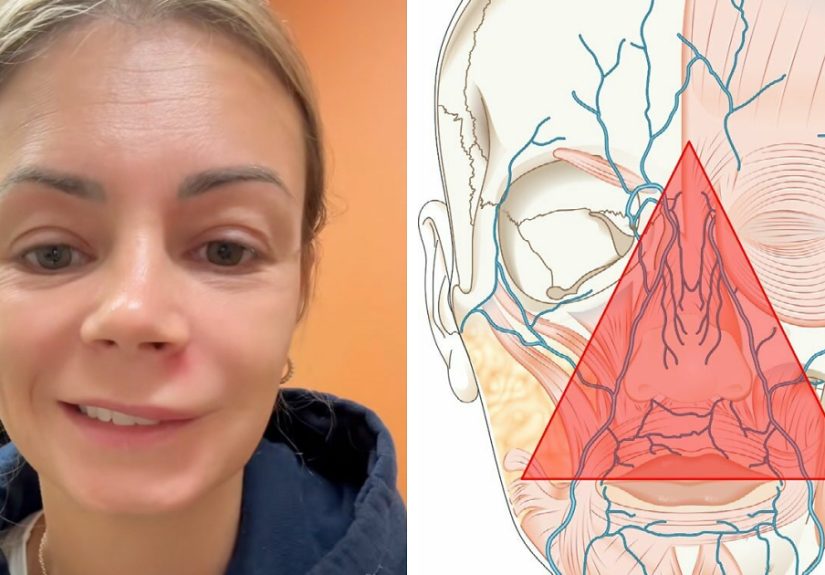
What Exactly Is the “Triangle of Death” (AKA the Danger Triangle)?
The danger triangle of the face generally refers to the area from the bridge of the nose down to the corners of the mouth,
including the nose and upper lip. It’s also called the “triangle of death” because infections here have a (rare) route to spread inward
toward deeper structures.
Why this region is different
Facial veins in this area connect to veins that drain toward spaces near the brain. Unlike many veins elsewhere, some facial venous pathways can allow
blood (and, in unusual cases, bacteria) to move in ways that make “backward” spread possible. That’s why clinicians pay special attention
to infections in the mid-face, especially around the nose.
Translation: the skin around your nose isn’t a direct tunnel to your brain (despite what your group chat might claim), but it does have venous connections
that can make certain infections more dangerous if they escalate.
Why Popping a Pimple Can Backfire (Even Outside the Triangle)
Dermatologists discourage DIY popping for a few unglamorous reasons:
- You can push gunk deeper, increasing inflammation and making the blemish bigger and angrier.
- You break the skin barrier, giving bacteria an easy entrance.
- You raise the risk of scarring and long-lasting dark marks (post-inflammatory hyperpigmentation).
- You can spread bacteria from your hands to your face (and to neighboring pores), turning one pimple into a breakout.
In other words: your fingers are not sterile instruments, your nails are tiny daggers, and your mirror lighting is not an FDA-approved surgical lamp.
So What Can Go Wrong in the Danger Triangle?
Most popped pimples won’t cause anything beyond redness, swelling, and regret. But doctors warn about this area because when infections do spread,
the complications can be serious.
1) Cellulitis (a spreading skin infection)
If bacteria get into the deeper layers of skin, you can develop cellulitis, which may cause a warm, expanding red area, pain, and swelling.
Facial cellulitis is taken seriously because swelling can worsen quickly and the infection can spread.
2) Nasal vestibulitis or boils around the nose
Pimples in or near the nostrils can sometimes be related to infections of the nasal vestibule. These can be uncomfortable and occasionally develop into an abscess
that needs medical treatment.
3) The headline-grabber: septic cavernous sinus thrombosis (very rare, very serious)
Here’s the big reason the triangle gets its dramatic nickname. In extremely rare cases, infection can spread to a deep venous space called the
cavernous sinus, leading to septic cavernous sinus thrombosis (a clot associated with infection). This can cause severe symptoms
and requires urgent hospital-level evaluation and treatment.
Doctors watch for warning signs like fever, severe headache, swelling around the eyes, eye pain, double vision, trouble moving the eyes, and neurologic symptoms.
This isn’t meant to scare you into never touching your face again (though honestly, your skin would probably love that). It’s meant to explain why clinicians
don’t shrug off rapidly worsening infections in the mid-face.
How Common Is This, Really?
The terrifying complications make great headlines because they’re dramatic—but they’re also uncommon, especially with modern hygiene,
prompt care, and antibiotics. The danger triangle warning exists because:
- When complications happen, they can escalate fast.
- Early treatment matters a lot.
- It’s easier to prevent infection than to chase it once it spreads.
Think of it like wearing a seatbelt. Most drives end just fine. The seatbelt is for the rare day things go sideways.
Red Flags: When a Pimple Stops Being “Just a Pimple”
If you have a pimple (popped or not) in the triangle of death/danger triangle—or anywhere on your face—get medical care quickly if you notice:
- Rapidly spreading redness or swelling
- Fever, chills, or feeling ill
- Severe facial pain (especially worsening overnight)
- Swelling around the eyes, eyelid drooping, or eye pain
- Blurry vision, double vision, or trouble moving your eyes
- Severe headache, neck stiffness, confusion, or fainting
- Facial weakness or drooping
If you’re debating whether something is “serious enough,” here’s a decent rule: if your symptoms are escalating quickly or involve your eyes,
nerves, or fever, don’t wait it out.
What Urgent Care or the ER Might Do
Treatment depends on what clinicians see and how severe things look. Options may include:
- Antibiotics (topical, oral, or IV depending on severity)
- Drainage if there’s an abscess (done by professionals in sterile conditions)
- Evaluation for deeper infection if eye symptoms or neurologic symptoms are present
- Imaging and specialist consults in concerning cases
- Hospital treatment for rare complications like cavernous sinus thrombosis (often involving IV antibiotics and sometimes anticoagulation)
The goal is simple: stop the infection early, reduce inflammation, and prevent spread.
Safer Alternatives: How to Treat a Deep, Painful Pimple Without the Drama
If you feel the urge to pop, try one of these options first (your future self will thank you).
Warm compresses: the low-tech hero
A warm compress can help reduce discomfort and encourage a deep pimple to resolve on its own. Use a clean warm (not burning) cloth for about 10–15 minutes,
a few times per day. It’s not glamorous, but it’s effective and doesn’t involve turning your fingertips into bacterial delivery systems.
Spot treatments that actually make sense
Over-the-counter options can help, depending on your skin:
- Benzoyl peroxide helps reduce acne-causing bacteria.
- Salicylic acid can help unclog pores.
- Adapalene (a topical retinoid) can help prevent future clogs over time.
Go slow: irritation can worsen inflammation. If you’re using multiple actives, avoid piling them all on at once like you’re seasoning a steak.
Hydrocolloid patches: the “hands-off” hack
Hydrocolloid pimple patches can protect a spot from picking, absorb fluid from certain types of pimples, and create a better healing environment. They’re
especially helpful when your biggest problem is… you touching it every 11 minutes.
Dermatologist-level fixes for cystic acne
If you get deep, painful cysts (especially around the nose or upper lip), consider professional care:
- Sterile extraction (when appropriate)
- Cortisone injections that can flatten a cyst faster
- Prescription routines tailored to your acne type and skin tolerance
Why the Triangle of Death Warning Is Worth Respecting
The warning isn’t meant to turn every blemish into a medical thriller. It’s a reminder that:
- Facial infections can spread quickly.
- The mid-face has anatomy that makes doctors cautious.
- Picking and popping raises the risk of infection and scarring.
- Prompt care for red-flag symptoms can prevent serious outcomes.
So yes, you can keep living your life. Just don’t audition for “Grey’s Anatomy: Bathroom Edition” the next time a pimple shows up under your nose.
Conclusion: Keep the Popcorn, Skip the Pimple-Popping
A pimple in the triangle of death is usually still just a pimple. But popping it can open the door to infection, and in rare cases, that infection can
become dangerous fast. If you’ve already popped one and symptoms are worsening—especially with fever, spreading redness, eye symptoms, severe headache, or facial weakness—get medical care.
Otherwise, treat the spot gently, keep it clean, use warm compresses, and consider evidence-based acne treatments. Your skin (and your weekend plans) will be much happier.
Real-Life Experiences: of “I Wish I’d Known That”
If you ask a room full of adults about their most regrettable skincare decisions, you’ll hear the same confessions on repeat—usually delivered with the haunted
look of someone who once believed toothpaste could solve cystic acne.
One common experience goes like this: you feel a deep bump forming near your nose, right where every selfie camera seems to sharpen. It’s tender, it’s swollen,
and it has that ominous “I’m about to ruin your mood” vibe. You tell yourself you won’t touch it. Then you touch it. Then you touch it again because
it feels like there’s pressure, and pressure is basically an invitation, right?
People describe the moment of popping as a weird little victory—like you’ve conquered a tiny dragon. But the next day, the dragon returns with friends.
Suddenly, the area is redder, warmer, and more painful. Some folks report swelling that creeps outward, turning a small spot into a “why is my face doing this”
situation. That’s often when regret hits: not because the pimple existed, but because the squeezing turned inflammation into an actual problem.
Another familiar story is the “important event ambush.” A wedding, a job interview, a first date—the pimple arrives on schedule like it has a calendar.
The temptation to pop spikes because you’re imagining photos forever. Ironically, that’s the exact moment when popping is most likely to create a scab, swelling,
or bruised discoloration that’s harder to hide than the original blemish. People later say they wish they’d used a warm compress, a pimple patch, or even booked a
quick dermatologist visit instead of trying to force a miracle with their fingernails.
Then there’s the group that learns the “danger triangle” lesson the hard way: they pop something near the upper lip or nose, and the aftermath feels
disproportionate—throbbing pain, swelling, maybe even pressure around the sinuses. Most of the time it resolves with proper care, but the anxiety is real. Once you’ve
spent an evening Googling symptoms while holding an ice pack to your face, you develop a new appreciation for the phrase “hands off.”
The most useful thing people say afterward isn’t “never get acne” (because, please). It’s “have a plan.” Keep gentle cleanser on hand.
Use evidence-based spot treatments. Stock a few hydrocolloid patches. And if you’re prone to deep, painful breakouts, treat it like a health issue, not a personal failure.
A dermatologist can often reduce the frequency and severity of these flare-ups, which means fewer moments where you’re negotiating with yourself in front of the mirror.
Bottom line from the lived-experience club: popping feels productive for about 12 seconds. Healing well feels better for weeks.