Table of Contents >> Show >> Hide
- First, What Exactly Is Plaque Psoriasis?
- Why Psoriasis Can Look Different on Darker Skin
- Myths & Facts: Plaque Psoriasis in People of Color
- Myth #1: “People of color don’t get psoriasis.”
- Myth #2: “If it isn’t bright red, it isn’t psoriasis.”
- Myth #3: “Those dark patches mean the psoriasis is gone.”
- Myth #4: “Psoriasis is contagious.”
- Myth #5: “It happens because you don’t wash enough.”
- Myth #6: “Scrub the scale off and you’ll fix it.”
- Myth #7: “If it’s not itchy, it’s not psoriasis.”
- Myth #8: “Phototherapy is always a perfect, no-downside option.”
- Myth #9: “Treatment is identical for everyone, so skin tone doesn’t matter.”
- Myth #10: “Biologics are only for extreme casesand they’re too risky.”
- When Psoriasis Is Missed: Why Accurate Diagnosis Can Take Longer
- Treatment Basics (with Skin-of-Color Realities Included)
- Barriers People of Color Report (and How to Push Back)
- Bottom Line: The Facts to Remember (Even on a Bad Skin Day)
- Experiences People Share (Composite Stories & Real-World Patterns)
- Conclusion
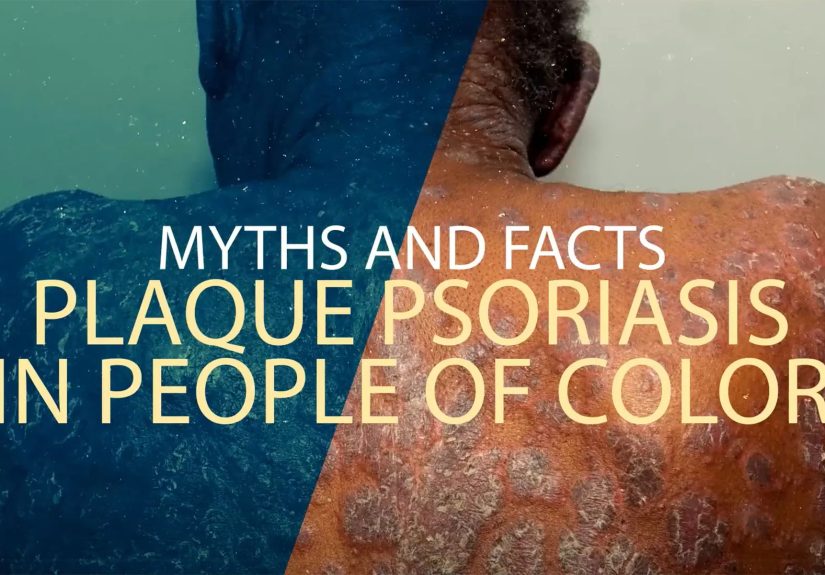
If you’ve ever tried to describe plaque psoriasis using the classic textbook phrase “red patches with silvery scale,”
and thought, “Cool, but my skin is not a textbook”welcome. Plaque psoriasis shows up in people of every
skin tone, but it doesn’t always show up in the same color palette. On darker skin, psoriasis can look violet,
grayish, deep brown, or even “where did it go?” until the light hits it just right.
This matters because when something is harder to recognize, it’s easier to mislabel, ignore, or “treat for a while and see.”
And with psoriasis, delays can mean more discomfort, more frustration, and more lingering pigment changes after the flare calms down.
So let’s do a myth-busting, fact-checking tourfocused specifically on plaque psoriasis in people of colorso you can spot
misinformation faster than psoriasis can build a layer of scale.
Quick note: This article is for education, not a diagnosis. If you think you have psoriasis (or you’re not sure),
a dermatologist can help confirm itsometimes with a close exam of the skin, scalp, and nails, and occasionally with a small biopsy.
First, What Exactly Is Plaque Psoriasis?
Plaque psoriasis is the most common type of psoriasis. It’s a chronic, immune-mediated condition that speeds up skin-cell turnover,
leading to raised, well-defined patches (plaques) with scale. It often shows up on the elbows, knees, scalp, trunk, and lower back,
but it can appear almost anywhereincluding the face, hands, and feet.
Psoriasis is also a “more than skin” situation. Some people develop psoriatic arthritis (joint pain, stiffness, swelling),
and psoriasis can significantly affect sleep, mood, and quality of life.
Two truths that kill a lot of myths
- Psoriasis is not contagious. You cannot catch it from touching, sharing towels, swimming pools, or close contact.
- Psoriasis isn’t caused by being “dirty.” The scale is not grime you can scrub away; it’s part of the inflammatory process.
Why Psoriasis Can Look Different on Darker Skin
Psoriasis involves inflammation, and inflammation can look different depending on how much melanin is in the skin.
On lighter skin, inflammation often reads as pink or red. On darker skin, the same inflammation may look violet,
purple, gray, or deep brownand sometimes the redness is simply less obvious.
The National Psoriasis Foundation notes that, on darker skin types, plaques may appear salmon, dark brown, purple, or violet
with a grayish scale, and that people of color may experience more dyspigmentation (hyperpigmentation or hypopigmentation)
with less visible redness.
The “after image” is real: dyspigmentation after flares
When plaques calm down, many people with medium-to-deep skin tones notice lighter or darker patches where the psoriasis used to be.
Dermatologists often call this dyspigmentation. It’s not a scar, but it can take time to fadesometimes 3 to 12 months or longer.
Treatment may be similar, but the experience isn’t identical
Major treatment categories are similar across skin tonestopicals, phototherapy, and systemic medsbut practical considerations can differ.
For example, phototherapy can darken skin or make dark spots more noticeable, and scalp treatment needs to fit real hair-care routines and textures.
Myths & Facts: Plaque Psoriasis in People of Color
Myth #1: “People of color don’t get psoriasis.”
Fact: People of all skin tones can develop psoriasis. Some U.S. prevalence estimates appear lower in certain racial/ethnic groups,
but major patient organizations emphasize that psoriasis can be under-identified on darker skin and misidentified as other conditions.
Translation: it’s not that psoriasis “skips” melaninit’s that the health system sometimes skips accurate recognition.
Myth #2: “If it isn’t bright red, it isn’t psoriasis.”
Fact: On darker skin, plaques may look violet, purple, grayish, or dark brown, and the scale can look gray instead of silvery.
The disease is the same; the color cues change.
Think of it like this: psoriasis didn’t changeyour skin’s “background color” just changes how inflammation shows up on camera.
Myth #3: “Those dark patches mean the psoriasis is gone.”
Fact: Darker (or lighter) areas after a flare can be dyspigmentation. It may fade slowly over months.
Sometimes the psoriasis is fully calm while pigment lingers; other times there’s still low-level activity.
If you’re unsure, a dermatologist can tell the difference and adjust treatment.
Myth #4: “Psoriasis is contagious.”
Fact: Psoriasis is not contagiousfull stop. You can’t “catch” it from contact, pools, towels, hugs, or sharing a bed.
It involves immune system activity and genetics, not a germ you pass around.
If anyone treats you like you’re contagious, that’s not “caution.” That’s misinformation wearing a trench coat.
Myth #5: “It happens because you don’t wash enough.”
Fact: Psoriasis isn’t caused by poor hygiene. The scale is part of the inflammatory process.
Over-washing and scrubbing can actually irritate skin and make flares harder to control.
Myth #6: “Scrub the scale off and you’ll fix it.”
Fact: Aggressive rubbing or “power-scrubbing” can worsen irritation and may contribute to hyperpigmentation,
especially in skin of color. Skin trauma can also trigger new plaques in some people (a phenomenon dermatologists call Koebnerization).
Gentle softening (think moisturizers, scale softeners, and doctor-guided treatments) is safer than a sandpaper approach.
Myth #7: “If it’s not itchy, it’s not psoriasis.”
Fact: Psoriasis can itch, burn, sting, feel tight, or sometimes feel like “nothing much” until it flares.
Symptom intensity varies person to person and flare to flare.
Myth #8: “Phototherapy is always a perfect, no-downside option.”
Fact: Phototherapy can be very effective, but for people with darker skin, it may darken treated areas or make pigment changes more noticeable.
That doesn’t mean it’s off the tableit means it should be a shared decision with realistic expectations and a plan for monitoring.
Myth #9: “Treatment is identical for everyone, so skin tone doesn’t matter.”
Fact: The treatment “menu” may be similar, but the practical choices can differ.
Vehicle matters (ointment vs. foam vs. oil vs. solution), especially for scalp psoriasis and different hair textures and wash schedules.
Discussing cultural hair-care routines isn’t “extra”it’s how treatment becomes realistic.
Myth #10: “Biologics are only for extreme casesand they’re too risky.”
Fact: For moderate-to-severe plaque psoriasis, systemic treatments (including biologics) can be life-changing and are widely used under medical supervision.
They’re not “casual meds,” but they’re also not automatically “last resort.” The right choice depends on severity, body areas affected, other health conditions,
and how much psoriasis affects your daily life.
A separate (and important) truth: organizations and researchers have documented gaps in access, representation, and comfort with advanced therapies among different groups,
which is why patient education and shared decision-making matter so much.
When Psoriasis Is Missed: Why Accurate Diagnosis Can Take Longer
Psoriasis in skin of color can be mistaken for other conditionsespecially when redness is less obvious, plaques look more violet/brown,
or pigment changes are the most visible feature. The NPF notes psoriasis on darker skin may resemble eczema, lichen planus, sarcoidosis,
discoid lupus, and other inflammatory conditions; sometimes clinicians use a biopsy to confirm.
How to advocate for a clearer answer (without becoming your own dermatologist)
- Bring photos of flares in different lighting and stages (early, peak, and “after”). Pigment changes can outlast redness.
- Ask about scalp and nailspsoriasis often shows clues there (flaking scalp, nail pitting or thickening).
- Use the “biopsy question”: “If you’re not certain, would a small biopsy help confirm the diagnosis?”
- Consider a dermatologist with skin-of-color experience, especially if you’ve had repeated “maybe eczema?” visits.
Treatment Basics (with Skin-of-Color Realities Included)
Psoriasis care usually stacks strategies: calm the inflammation, reduce scale, protect the skin barrier, and prevent flares.
Most plans mix medical treatment with daily habits that make skin less reactive.
1) Topicals: the “front line” for many people
Topical corticosteroids, vitamin D analogs, retinoids, and other anti-inflammatory creams/ointments are common starting points.
The goal is controlled use: strong enough to calm plaques, smart enough to avoid side effects from overuse.
Skin-of-color tip: If your main frustration is the “shadow” left behind after flares, don’t self-treat pigment with harsh brighteners.
First priority is controlling inflammation (so pigment doesn’t keep getting triggered). Then your clinician can help with safer options.
2) Scalp psoriasis: where real life meets medical life
Scalp plaques can be stubborn because hair makes application harder and daily medicated shampoo use may not match everyone’s hair-care routine.
Dermatology literature notes that vehicle choice (oils, foams, solutions) can improve adherence in patients with certain hair textures and styles.
- If daily shampooing feels impossible or damaging, ask about non-shampoo options (foams, oils, leave-on solutions).
- Be gentle with scratchingskin trauma can trigger more plaques, and aggressive scratching can worsen pigment changes.
3) Phototherapy: effective, but discuss pigment expectations
Phototherapy (often narrowband UVB) can slow the overactive skin-cell cycle and reduce inflammation.
For people with darker skin, it may cause tanning/darkening or make dark spots more noticeable, so talk through cosmetic priorities and monitoring.
4) Systemic meds and biologics: when psoriasis is more than “a few spots”
If plaques cover a larger body area, involve high-impact locations (hands, feet, face, genitals), or significantly affect life,
clinicians may recommend oral or injected medications that treat inflammation from the inside out.
The point isn’t “graduating” to stronger meds as a moral achievement. The point is matching treatment intensity to disease burden.
Many people of color report feeling dismissed because plaques “don’t look that red.” But severity isn’t only colorit’s thickness, scale,
body area, symptoms, and how much it disrupts your life.
Barriers People of Color Report (and How to Push Back)
Patient resources emphasize that people of color can face barriers to accurate diagnosis and treatmentranging from under-recognition of psoriasis
on darker skin to access issues and limited representation in educational images.
Practical “push back” strategies
- Name the concern clearly: “I’m worried this looks different on my skin tone. Can we confirm psoriasis vs. eczema vs. fungal causes?”
- Ask for a plan with checkpoints: “If this treatment doesn’t improve in 2–4 weeks, what’s our next step?”
- Use reputable patient tools: national organizations maintain education and provider resources for psoriasis and skin of color.
- Track triggers: stress, infections, skin injury, and other factors can worsen flares; pattern-spotting helps your clinician personalize care.
Bottom Line: The Facts to Remember (Even on a Bad Skin Day)
- Plaque psoriasis affects all skin tones, but it may not look “red” on darker skin.
- It is not contagious, and it is not caused by poor hygiene.
- After a flare, pigment changes can linger for monthsoften longer than the plaque itself.
- Effective treatments exist; the best plan is the one you can actually follow (especially for scalp care).
Experiences People Share (Composite Stories & Real-World Patterns)
The stories below are composite experiencesbased on common themes reported in patient education resources and dermatology discussions,
not on any single identifiable person. The goal is to make the “myths vs. facts” feel less like a quiz and more like real life.
1) “They kept calling it eczema… until it didn’t act like eczema.”
A common frustration among people with deeper skin tones is the “diagnosis merry-go-round.” Someone notices thick, scaly patches that look
violet-brown rather than bright red. Because the classic redness isn’t obvious, they’re told it’s eczema, a fungal rash, or “just dryness.”
They try moisturizers, maybe a mild steroid, maybe an antifungal shampoosome things help a little, but the plaques keep returning in the same places,
with the same stubborn scale.
The turning point is often a visit with a clinician who looks beyond color:
Are the borders sharp? Is there thick scale? Are there scalp or nail clues? Sometimes a quick biopsy seals the deal.
Once the person finally gets a clear plaque psoriasis diagnosis, the emotional reaction is oddly mixed: relief (“I’m not imagining this”)
and anger (“Why did it take so long?”). That’s when myth #1 (“people of color don’t get psoriasis”) shows its real-world damage: it can quietly
slow down recognition and treatment.
2) “The plaques faded… but the dark marks stayed and stole the spotlight.”
Many people with medium-to-dark skin say the most stressful phase isn’t always the flareit’s the aftermath.
The plaque calms down, the scale softens, the itching improves… and then pigment changes remain like a stubborn souvenir.
Friends and family may assume the condition is still “active” because they can still see the darker areas.
The person may feel stuck explaining, “It’s not infectious,” “It’s not dirty,” and “No, I can’t scrub it off.”
This is where it helps to separate inflammation control from pigment recovery.
People often report that when treatment is consistent early (instead of delayed or on-and-off),
the pigment changes seem less intense and clear sooner. They also learn to avoid over-scrubbingbecause irritation can deepen hyperpigmentation.
It’s a slow-win strategy: calm the immune flare first, then support the skin barrier and let pigment normalize over time.
3) “Scalp psoriasis collided with wash-day reality.”
Scalp psoriasis has a special talent for being loud at the worst times: big meeting, family photo, fresh braids, new twist-out.
People of color often describe a gap between the instructions they receive (“use this medicated shampoo daily”)
and what’s realistic for their hair type, protective styles, or wash schedule. When the plan doesn’t fit real life,
adherence dropsand then the clinician may assume the medication “failed.”
In better experiences, the conversation is more practical: switching to foam, oil-based solutions, or leave-on treatments;
talking about how to apply medication without disrupting styles; and setting expectations (“we’re reducing inflammation first,
then managing scale”). People frequently say that once the treatment fits their routine, they’re finally able to stay consistent
and consistency is where psoriasis management starts to feel possible again.
4) “I didn’t want to ‘escalate’ treatmentuntil I realized how much psoriasis was stealing from my day.”
Another common theme is hesitation around systemic medications. Some people worry that biologics or oral meds are “too intense,”
or they feel they haven’t “earned” themlike psoriasis care is a weird merit badge system. But after months (or years) of flares,
sleep disruption, visible plaques in high-impact areas, and the mental load of constant explaining, many people reframe the decision:
the risk of doing nothing is also a risk.
People who report better outcomes often describe a similar pattern: they learned the facts (psoriasis is immune-mediated, not contagious),
they asked direct questions about safety monitoring, and they chose a plan that matched their severity and lifestyle.
The biggest “experience-based” lesson is simple: you deserve treatment that reflects your burdennot just how red the plaques look.
Conclusion
Plaque psoriasis in people of color is a masterclass in why “one-size-fits-all visuals” fail. The myths are loud“it’s contagious,”
“it’s poor hygiene,” “psoriasis is always red”but the facts are stronger: psoriasis affects every skin tone, can look violet or brown on darker skin,
and may leave pigment changes that linger long after the plaque improves.
If there’s one takeaway worth taping to your bathroom mirror (next to the moisturizer), it’s this:
you’re allowed to ask for clarity. Ask for confirmation. Ask about biopsy. Ask about scalp-friendly vehicles.
Ask about pigment expectations. Myths thrive in silence; psoriasis management thrives in specifics.







