Table of Contents >> Show >> Hide
- First: How “Risky” Was It, Really?
- Emergency Contraception: Your “Undo” Button (With a Time Limit)
- When to Take a Pregnancy Test (Without Torturing Yourself)
- The Emotional Side: Panic Is Normal, But It’s a Terrible Project Manager
- Prevention: How to Avoid the Next Pregnancy Scare
- Quick FAQ
- Conclusion
- Real Experiences: What a Pregnancy Scare Often Looks (and Feels) Like
- 1) “The condom broke, and now I’m counting minutes like it’s a spy movie.”
- 2) “I took emergency contraception… and now every twinge is a ‘symptom.’”
- 3) “I tested early. It was negative. I felt better for an hour… then panicked again.”
- 4) “I was scared to tell anyone, but secrecy made it 10x worse.”
- 5) “After it was over, I promised myself: never again.”
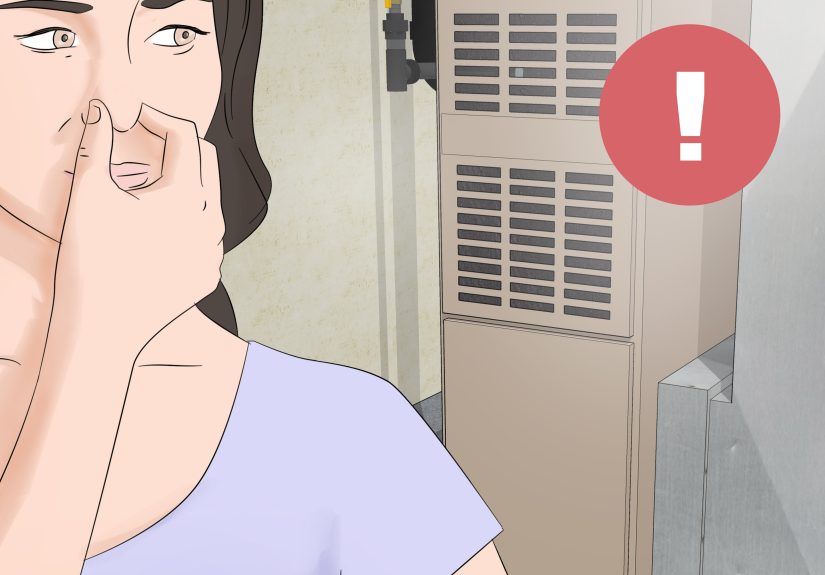
A pregnancy scare can feel like your brain opened 37 tabs at onceeach one screaming “WHAT IF?!”
If you’re here because something didn’t go as planned (missed pill, condom slip, timing confusion, or a
full-on “we’ll be careful” moment), take a breath. There are practical steps you can taketodayand
they’re a lot more effective than panic-refreshing your calendar app.
This guide covers what to do right away (including emergency contraception), when and how to take a pregnancy test,
how to handle the emotional spiral, and how to prevent a repeat performance. Friendly reminder: this is educational,
not personal medical advicewhen in doubt, a pharmacist or clinician can help you choose the best option.
First: How “Risky” Was It, Really?
Not every scare has the same odds. Pregnancy can only happen if sperm is present and ovulation timing lines up.
That said, real life is messy, cycles vary, and stress doesn’t exactly come with a built-in math calculator.
Common situations that can lead to a pregnancy scare
- Sex without contraception (or starting late)
- A condom breaks, slips off, or is used incorrectly
- Missed birth control pills (especially early in the pack) or delays with patch/ring/shot
- “Withdrawal” timing errors (it’s not as reliable as people think)
- Sex around your fertile window when cycles are irregular
If any of that sounds familiar, the best move is to shift into “next step” mode: emergency contraception (if you’re within the window),
then a testing plan, and then prevention so you don’t have to live in Suspense: The Musical ever again.
Emergency Contraception: Your “Undo” Button (With a Time Limit)
Emergency contraception (EC) helps prevent pregnancy after sex but before pregnancy starts.
EC works mainly by delaying or preventing ovulation. The key phrase is: the sooner, the better.
The main emergency contraception options in the U.S.
| Option | How fast you need it | Pros | Things to know |
|---|---|---|---|
| Levonorgestrel pill (Plan B One-Step and generics) |
Best within 72 hours (3 days); can work up to 120 hours (5 days) | Over-the-counter, widely available, simple one-dose option | Less effective the longer you wait; may be less effective at higher body weights |
| Ulipristal acetate pill (ella) |
Works up to 120 hours (5 days) and stays effective across that window | Often more effective than levonorgestrel, especially closer to day 5 | Prescription required; you’ll need to delay starting hormonal birth control for a few days afterward |
| Copper IUD (inserted by a clinician) |
Can be inserted within 5 days (sometimes even later depending on ovulation timing) | Most effective EC option; becomes long-term birth control for years | Requires an appointment and insertion; may increase cramps/bleeding for some people |
Which one should you choose?
If you can’t get everything, get something. The “best” EC is the one you can take soonestunless you have access to a clinician quickly,
in which case an IUD or prescription option may be a better fit.
-
If it’s been 0–3 days: Levonorgestrel is often easiest to access quickly. If you can get ella in time,
it may be more effective. - If it’s been 4–5 days: ella or a copper IUD is usually a stronger choice because levonorgestrel’s effectiveness drops as time passes.
-
If body weight is a concern: Some evidence suggests levonorgestrel (and possibly ella) may be less effective at higher weights,
while IUDs remain highly effective regardless of weight.
What to expect after taking emergency contraception
EC can nudge your cycle around. That doesn’t mean it “didn’t work.” It means hormones are doing hormone things.
Some common short-term effects include:
- Nausea or upset stomach
- Headache, dizziness, or fatigue
- Tender breasts
- Spotting or light bleeding
- Your next period coming earlier or later than usual
Consider checking in with a clinician promptly if you have severe abdominal pain, very heavy bleeding, or symptoms that worry you.
(Also: if you vomit soon after taking a pill, ask a pharmacist or clinician what to do next.)
Starting (or restarting) regular birth control after EC
A smart move after a scare is making sure you’re protected going forward.
-
After levonorgestrel EC: you can usually start or resume hormonal birth control right away,
but use condoms/backup for a short window while your regular method becomes effective. -
After ella (ulipristal acetate): you’ll typically be advised to wait several days before starting hormonal birth control,
and use condoms/backup in the meantime.
If this part feels confusing, you’re not alone. A pharmacist, clinic, or prescribing provider can give you a simple, personalized “start date + backup plan.”
When to Take a Pregnancy Test (Without Torturing Yourself)
Here’s the frustrating truth: testing too early is a common reason people get a negative result and then spiral anyway.
Pregnancy tests detect a hormone called hCG, which rises after implantation. Translation: your body needs time to produce enough hCG to show up reliably.
Timing that’s actually helpful
- Most reliable: test after your missed period (or a day or two after).
-
Possibly detectable earlier: some tests can detect pregnancy about 10 days after conception,
but false negatives are more likely if you test early.
How to test smarter (and reduce false negatives)
- Use first-morning urine when possible (it’s more concentrated).
- Read directions carefully (different brands have different timing windows).
- Don’t “over-interpret” faint linesif unsure, repeat with a new test or get a clinic test.
-
If you test negative but your period still doesn’t come: test again in 48–72 hours, or within a week.
Many clinicians recommend retesting if your period is late by a week.
After emergency contraception: when should you test?
Because EC can shift your cycle, focus on a simple rule: test if your period is significantly late or unusual.
If you took ella and don’t get a period within a few weeks, take a pregnancy test.
If the test is positive (or you’re not sure)
Take a second test to confirm, ideally with a different brand, or schedule a clinic test. If you have pain, heavy bleeding,
or feel unwell, seek medical care promptly. If you need to talk through options, many clinics can provide confidential, nonjudgmental support.
The Emotional Side: Panic Is Normal, But It’s a Terrible Project Manager
Pregnancy scares aren’t just about biologythey’re about pressure, uncertainty, and the feeling that your entire future is waiting behind one tiny plastic stick.
If you’re anxious, you’re not “dramatic.” You’re human.
Common feelings people report
- Fear (“I’m not ready.”)
- Guilt (“I should’ve been more careful.”)
- Anger (“Why is this on me?”)
- Shame (“I can’t tell anyone.”)
- Hypervigilance (Googling symptoms like it’s a second job)
Ways to calm the spiral (that don’t involve doom-scrolling)
-
Make a plan in writing: “EC today, test on X date, backup protection until Y, clinic call if Z.”
A plan is the opposite of panic. -
Set a “Google curfew”: Give yourself 10 minutes to look up reputable info, then stop.
(Yes, Reddit has feelings. No, it is not your doctor.) -
Tell one safe person: A trusted friend, sibling, counselor, or clinic staff member.
Keeping it secret often magnifies stress. -
Do something physical: Walk, stretch, shower, breathe slowly for 2 minutes.
Your nervous system needs a signal that you’re safe.
If your anxiety feels unmanageablecan’t sleep, can’t eat, constant intrusive thoughtsreach out to a healthcare professional or counselor.
You deserve support for the emotional part, too.
Prevention: How to Avoid the Next Pregnancy Scare
The goal isn’t perfection. The goal is fewer “oh no” moments and more “we’ve got this” systems.
Think of prevention like a seatbelt: you don’t plan to crash, you just prefer not to find out what the dashboard tastes like.
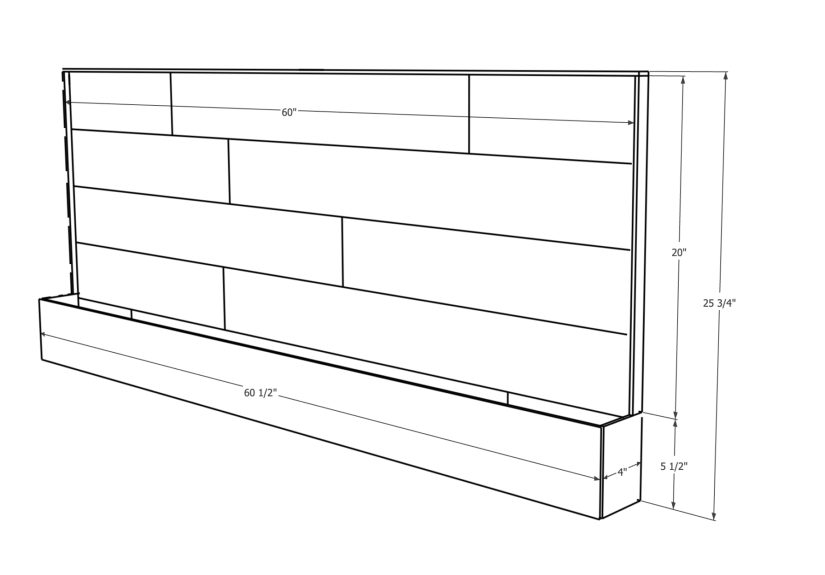
Build a two-layer protection habit
- Layer 1 (pregnancy prevention): a reliable birth control method that matches your life (pill, patch, ring, shot, implant, IUD).
- Layer 2 (STI protection): condoms (internal or external). Condoms also help as backup if you miss a dose or start late.
Make your method easier to use (because life is chaotic)
- Set reminders for pills/patch/ring changes.
- Keep condoms visible (not buried like a time capsule).
- Refill early so you’re not rationing pills like they’re rare collectibles.
- Consider long-acting reversible contraception (LARC) like an implant or IUD if you want “set it and forget it” protection.
Create a “just in case” plan
A lot of pregnancy scares are scary because people aren’t sure what to do next. You can fix that ahead of time:
- Know where you’d go (pharmacy, clinic, telehealth) for EC or questions.
- Know what you’d do for a test (buy one, clinic visit, when to test).
- Know what backup method you’ll use for the next 7 days if your routine method gets off track.
Bonus prevention: protect your peace
Prevention isn’t only physicalit’s emotional. Clear communication, consent, and shared responsibility matter.
If you feel pressured or unsafe, that’s not a “contraception problem.” That’s a relationship and safety problemand you deserve better.
Quick FAQ
Does emergency contraception cause an abortion?
Emergency contraception helps prevent pregnancy from starting, mainly by delaying ovulation. It does not end an established pregnancy.
Can I use emergency contraception more than once?
It’s generally considered safe for repeated use, but it’s not as effective (or as chill for your cycle) as a consistent birth control method.
If you’ve needed EC more than once, that’s a good sign to upgrade your routine plan.
Should I worry about STIs after a scare?
EC prevents pregnancy, not infections. If you had sex without barrier protection, consider STI testing based on your situation.
Many clinics can guide you on timing and the right tests.
Conclusion
A pregnancy scare can be intensebut you’re not powerless. Acting quickly (when possible), testing at the right time,
and building a prevention plan can turn “I’m freaking out” into “I’m handling it.”
If you remember nothing else, remember this: speed helps with emergency contraception, timing helps with pregnancy tests,
and support helps with everything. You don’t have to carry the stress alone.
Requirement #7: Add ~ of experiences at the end
Real Experiences: What a Pregnancy Scare Often Looks (and Feels) Like
People talk about pregnancy scares like they’re purely logisticaltake a pill, take a test, move on. But in real life, it’s usually more emotional,
more awkward, and more “why is my brain doing this” than anyone admits. Here are some common, relatable experiences people describeshared as
composite scenarios so you can see yourself in them without putting anyone’s private life on display.
1) “The condom broke, and now I’m counting minutes like it’s a spy movie.”
This is the classic adrenaline surge: sudden realization, instant fear, and a weird urge to re-live the moment in slow motion to determine if it “counts.”
What helps most here is action. Many people say their anxiety drops the second they get emergency contraception in handbecause uncertainty shrinks when a plan exists.
A common follow-up feeling is second-guessing: “Was it too late?” The reality is that acting quickly is genuinely useful, so most people feel relief knowing
they did the best possible thing in the moment.
2) “I took emergency contraception… and now every twinge is a ‘symptom.’”
After EC, it’s normal to notice your body more than usual. Some people report checking for spotting, tracking cramps, or reading into changes in discharge.
The tricky part is that EC itself can cause temporary side effects and cycle changesso the body signals you’re monitoring may be from the medication,
stress, or your normal cycle. Many people say it helps to pick one trustworthy source of information, write down expected side effects, and then stop
symptom-hunting like it’s a competitive sport.
3) “I tested early. It was negative. I felt better for an hour… then panicked again.”
Testing early can create a roller coaster: a negative result feels like instant freedomuntil you remember, “Wait… was it too early?”
A common lesson people share is that testing works best when timed well. The most calming approach is often a testing schedule:
pick a date around a missed period (or later if cycles are irregular), test with first-morning urine, and decide ahead of time what you’ll do
if the result is negative but your period doesn’t show up (usually: retest after a couple days or within a week).
4) “I was scared to tell anyone, but secrecy made it 10x worse.”
Many people describe the stress peaking when they feel isolatedespecially if they worry about judgment. The turning point is often telling one safe person:
a close friend, a trusted adult, a counselor, a clinic staff member, or even a pharmacist who treats it like the everyday healthcare question it is.
The most repeated quote (paraphrased) is basically: “No one yelled. No one fainted. I built it up in my head.”
5) “After it was over, I promised myself: never again.”
A lot of people come out of a scare with a new respect for preventionless out of shame, more out of self-protection.
They switch to a method that’s easier to use, set reminders, keep condoms accessible, or choose a longer-acting option so they’re not relying on
perfect timing every month. The healthiest version of “never again” isn’t punishmentit’s a practical upgrade:
“I deserve a plan that doesn’t require me to be flawless.”
If you’re in the middle of a scare right now, the biggest takeaway from others’ experiences is simple:
you will feel better once you take concrete steps. Even one stepgetting EC, choosing a test date, or talking to a cliniccan turn
the volume down on the panic. And if you’ve already taken steps? That’s not “too little.” That’s you showing up for yourself.