Table of Contents >> Show >> Hide
- Meet the villain: what ragweed is (and why it’s so good at annoying you)
- Ragweed allergy symptoms: what it feels like in real life
- When does ragweed season hit?
- Is it ragweed allergies… or a cold?
- Why your body reacts: the 60-second immune explanation
- How ragweed allergies are diagnosed
- Treatment that actually works: a practical “step-up” game plan
- Step 1: Reduce exposure (without becoming a full-time indoor person)
- Step 2: Over-the-counter medications (the “don’t suffer unnecessarily” toolkit)
- 1) Intranasal corticosteroid sprays (often the MVP)
- 2) Antihistamines (oral or nasal)
- 3) Eye drops for itchy, watery eyes
- 4) Decongestants (use carefully)
- 5) Saline irrigation and supportive care
- Step 3: Prescription options for stubborn symptoms
- Step 4: Immunotherapy (long-term treatment, not just symptom cover-up)
- Allergy shots (subcutaneous immunotherapy)
- Sublingual immunotherapy (SLIT) tablets for ragweed
- Ragweed + food: why melons sometimes bite back
- When to see a clinician (and when to seek urgent care)
- A simple “pre-season” strategy that helps a lot of people
- Real-world experiences: what ragweed season is actually like (and what tends to help)
- SEO Tags
Ragweed is the overachiever of the weed world. It doesn’t have pretty flowers. It doesn’t smell nice. It doesn’t even
contribute to your fall aesthetic. What it does do is release microscopic pollen that can turn late summer and
early fall into a season-long audition for “Best Sneezing Sound Effects.”
If your nose starts acting like it’s offended by oxygen every August, you’re not imagining it. Ragweed allergy is a
major cause of seasonal allergic rhinitis (aka hay fever), and it can trigger symptoms from mild sniffles to full-on
“why are my eyes leaking?” misery. The good news: there are proven treatmentsand a few practical tricksthat can make
ragweed season a lot more livable.
Quick note: This article is for education, not a substitute for personal medical advice. If you have
asthma, severe symptoms, or questions about medications, a clinician or allergist can tailor a plan for you.
Meet the villain: what ragweed is (and why it’s so good at annoying you)
Ragweed is a group of plants (common ragweed and giant ragweed are the usual suspects) that thrives in vacant lots,
roadsides, fields, and anywhere humans have disturbed soil. The plant’s pollen is lightweight and designed for wind
travelso it doesn’t just bother people standing next to a patch of weeds. It can spread through the air for long
distances, which is why you can feel symptoms even if you don’t see ragweed in your neighborhood.
The immune system part is the real plot twist: with ragweed allergy, your body mislabels ragweed pollen as a threat,
then overreacts. That reaction releases chemicals (like histamine) that create the classic allergy symptoms.
Ragweed allergy symptoms: what it feels like in real life
Ragweed allergy symptoms can overlap with a cold, but the pattern is usually the giveaway: symptoms show up during
ragweed season, get worse outdoors or on high-pollen days, and may improve when you’re inside with filtered air.
Nose and throat symptoms
- Sneezing (sometimes in dramatic, unstoppable streaks)
- Runny nose or postnasal drip
- Stuffy nose (congestion that makes you sound like you’re talking through a pillow)
- Itchy nose, itchy throat, or scratchy throat
- Cough from postnasal drip (especially at night)
Eye symptoms (allergic conjunctivitis)
- Itchy, watery eyes
- Redness and irritation
- Puffy eyelids (the “I swear I slept” look)
Chest symptoms and asthma flares
If you have asthma, ragweed pollen can trigger wheezing, chest tightness, cough, or shortness of breath. Even without
asthma, some people notice exercise feels harder during peak pollen weeks.
Skin symptoms (less common, but possible)
Some people get hives or a rash, especially if they’ve been in contact with the plant or have strong environmental
sensitivities.
“Allergy brain” and sleep disruption
Constant congestion and postnasal drip can wreck sleep, which can translate into fatigue, irritability, and that fuzzy
“why can’t I focus?” feeling. Not fun. Also not your fault.
When does ragweed season hit?
In much of the U.S., ragweed season typically starts around August, peaks in mid-September,
and can continue into Octoberoften lasting until the first hard frost knocks the plant out.
In some regions, it can run into November. The exact timing depends on where you live and what the weather is doing.
Translation: you can be perfectly fine in July, then suddenly become allergic to “outside” in late summer.
If you track your symptoms on a calendar, you’ll often see the same story repeat every year.
Is it ragweed allergies… or a cold?
Because the universe loves confusion, ragweed allergy symptoms can mimic a respiratory virus. Here’s a practical way
to tell them apart:
- Allergies often cause itching (eyes/nose), sneezing, and clear drainage.
- Colds often come with a sore throat early on, thicker mucus over time, and usually resolve in about a week or two.
- Fever and body aches are more typical of infections than allergies.
If symptoms persist for weeks and line up with ragweed season, allergies move to the top of the suspect list.
Why your body reacts: the 60-second immune explanation
With ragweed allergy, your immune system makes allergy antibodies (IgE) that recognize ragweed pollen. Next time you
breathe in pollen, those IgE antibodies trigger immune cells to release histamine and other chemicals. That’s what
leads to sneezing, itching, congestion, and watery eyes.
It’s not that you’re “weak.” It’s that your immune system is being a little too enthusiastic about the wrong target.
How ragweed allergies are diagnosed
Many people self-identify ragweed allergy because the timing is so consistent. But if symptoms are significantor if
you want a plan that actually worksformal diagnosis helps.
What a clinician may look for
- A seasonal pattern (late summer/fall symptoms)
- Triggers (worse outdoors, worse on high-pollen days, better indoors)
- Family history of allergies, asthma, or eczema
- Signs of allergic inflammation in the nose and eyes
Testing options
- Skin prick testing: tiny amounts of allergen are introduced to the skin to see if a reaction occurs.
- Blood testing (specific IgE): measures allergy antibodies to ragweed in the blood.
Testing is especially useful if you have asthma, frequent sinus issues, severe symptoms, or you’re considering
immunotherapy (allergy shots or sublingual tablets).
Treatment that actually works: a practical “step-up” game plan
Ragweed allergy treatment usually isn’t one magic trickit’s a smart combination. Think of it like building a
“pollen defense system” where each layer helps.
Step 1: Reduce exposure (without becoming a full-time indoor person)
- Check pollen forecasts and limit long outdoor time on high-count days.
- Keep windows closed during pollen season (home and car, especially on windy days).
- Shower and change clothes after being outdoorspollen sticks to hair, skin, and fabric.
- Rinse your nose with saline after outdoor exposure (especially if you feel “pollen-y”).
- Use HVAC filters and/or a HEPA air cleaner to lower indoor pollen levels.
- Dry laundry indoors during peak season when possible (outdoor drying can collect pollen).
- Consider a well-fitted mask for yard work or long outdoor activities during peak days.
Indoor air matters because you spend a lot of time there. A HEPA filter (in an air purifier or HVAC system) is designed
to capture tiny particlesincluding pollenso you’re not marinating in allergens at home.
Step 2: Over-the-counter medications (the “don’t suffer unnecessarily” toolkit)
These are common options; the best choice depends on whether your main issue is sneezing/itching, congestion, or eye
symptoms.
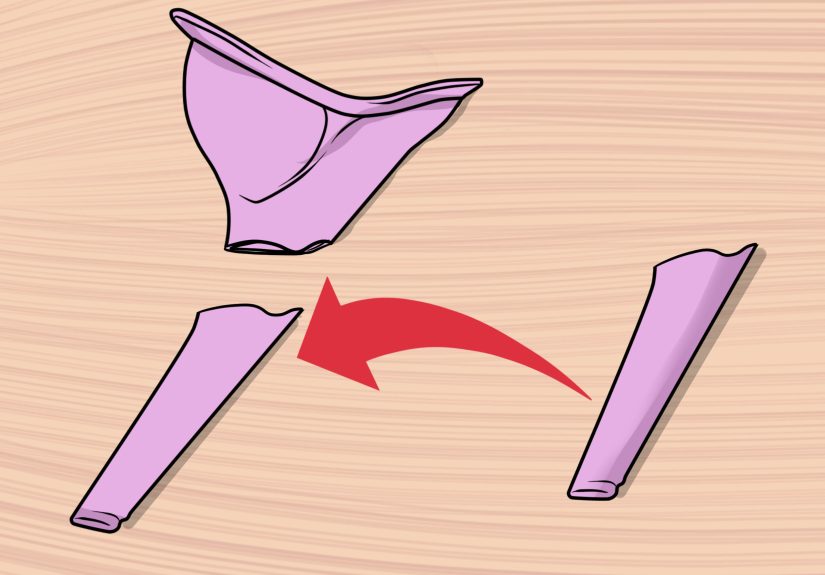
1) Intranasal corticosteroid sprays (often the MVP)
Nasal steroid sprays reduce inflammation and are among the most effective treatments for allergic rhinitisespecially
for congestion. They work best when used consistently during the season (not just once you’re already miserable).
Pro tip for technique: aim the spray slightly outward (away from the middle “wall” of your nose) and
sniff gently. This can lower the chance of irritation or nosebleeds.
2) Antihistamines (oral or nasal)
Antihistamines block histamine and can help with sneezing, itching, and runny nose. Non-drowsy options are popular for
daytime. Antihistamine nasal sprays can also help nasal symptoms and may work quickly.
3) Eye drops for itchy, watery eyes
Antihistamine eye drops can be a game-changer if your eyes are the main drama queens. If you wear contact lenses, check
product guidance and consider using drops before inserting lenses.
4) Decongestants (use carefully)
Decongestants can reduce stuffiness, but they’re not for everyone. Oral versions may raise blood pressure or cause
jitteriness. Nasal decongestant sprays should generally not be used for more than a few days in a row because they can
cause rebound congestion (the “I used it and now my nose is worse” phenomenon).
5) Saline irrigation and supportive care
Saline sprays or rinses can physically wash pollen out of your nasal passages. They won’t replace medication for
moderate-to-severe allergies, but they can lower the overall “allergen load” and help you breathe easier.
Step 3: Prescription options for stubborn symptoms
If you’ve tried the basics and still feel wrecked, it’s time to talk with a clinician. Prescription strategies may
include:
- Combination nasal sprays (for example, steroid + antihistamine formulations)
- Leukotriene receptor antagonists (sometimes used when allergies and asthma overlap; not first-line for everyone)
- Asthma controller adjustments if ragweed season reliably triggers wheezing or flare-ups
The goal isn’t “more meds.” The goal is the right meds in the right seasonso you can function like a
human again.
Step 4: Immunotherapy (long-term treatment, not just symptom cover-up)
If ragweed knocks you down every year, immunotherapy can help by training your immune system to be less reactive over
time. This is the closest thing allergy care has to a “long game” solution.
Allergy shots (subcutaneous immunotherapy)
Allergy shots deliver gradually increasing doses of allergen under medical supervision. Over time, many people have
fewer symptoms and need less medication. It typically requires a build-up phase followed by maintenance dosing over
several years.
Sublingual immunotherapy (SLIT) tablets for ragweed
A prescription ragweed tablet (taken under the tongue) is another option for certain people with confirmed ragweed
allergic rhinitis (with or without conjunctivitis). It’s commonly started well before ragweed season and continued
through the season. Because allergic reactions are possible, clinicians usually supervise the first dose and give
safety guidance.
Immunotherapy is especially worth discussing if you:
- Have symptoms that interfere with school, work, sleep, or exercise every fall
- Rely on multiple medications and still feel bad
- Have asthma that flares during ragweed season
- Prefer a long-term strategy rather than repeating the same seasonal struggle
Ragweed + food: why melons sometimes bite back
Some people with ragweed allergy notice itching or tingling in the mouth after eating certain raw fruits and veggies.
This is often called pollen food allergy syndrome (also known as oral allergy syndrome). It happens
because certain foods have proteins similar to pollen proteinsyour immune system gets confused and reacts.
Foods commonly associated with ragweed-related cross-reactivity can include banana, cucumber, melons
(like watermelon or cantaloupe), zucchini, and sometimes sunflower seeds.
The good news: symptoms are usually mild and limited to the mouth/throat, and cooking the food often reduces the
reaction because heat changes the proteins. The serious-news footnote: if symptoms feel severe, spread beyond the
mouth, or involve trouble breathing, get medical help.
When to see a clinician (and when to seek urgent care)
Make an appointment if:
- Symptoms last weeks and interfere with sleep, school, work, or exercise
- Over-the-counter meds aren’t enough (or you’re using them constantly)
- You have frequent sinus infections or persistent facial pressure
- You have asthma symptoms or wheezing during ragweed season
- You want testing and a long-term plan (including immunotherapy)
Seek urgent care right away if:
- You have trouble breathing, chest tightness that’s escalating, or severe wheezing
- You have signs of a severe allergic reaction (widespread hives, swelling of lips/tongue, dizziness)
- Your asthma rescue inhaler isn’t helping the way it normally does
A simple “pre-season” strategy that helps a lot of people
Here’s a surprisingly effective move: don’t wait for symptoms to get awful. If ragweed hits you every year,
start your prevention plan early.
Try this timeline
- 2–4 weeks before your usual flare: start your most effective baseline medication (often a nasal steroid spray).
- When pollen rises: add an antihistamine or eye drops if itching/sneezing ramps up.
- Peak weeks: tighten exposure steps (shower after outdoors, HEPA filtration, windows closed).
- If symptoms still break through: talk with a clinician about combination therapy or immunotherapy.
The goal is to keep inflammation from building like a slow-motion traffic jam. Once your nasal passages are fully
inflamed, it’s harder (and slower) to get relief.
Real-world experiences: what ragweed season is actually like (and what tends to help)
People often describe ragweed season as a “creeping start.” It begins with a tiny tickle in the nose that feels
harmlesslike maybe you slept near a dusty vent. Then, over a week or two, the symptoms stack up: sneezing in the
morning, watery eyes by afternoon, congestion at night, and the kind of fatigue that makes you wonder if you’re
secretly training for a nap marathon.
One common experience is the “outdoor-to-indoor whiplash.” Someone might feel okay while running errandsthen get home,
sit on the couch, and suddenly start sneezing. That’s often because pollen has hitched a ride on hair, skin, and
clothing. People who make one small changelike showering and changing clothes after time outsidefrequently report
fewer evening symptoms. It’s not glamorous, but it’s effective. (Ragweed is clingy. You have to set boundaries.)
Another theme: mornings can be rough. Many people notice symptoms spike after early commutes, school drop-offs, or
morning workouts. A practical workaround is shifting exercise indoors during the worst weeks, or wearing a mask for
outdoor chores like mowing, raking, or gardening. Folks who do yard work without protection often describe feeling fine
during the task, then paying for it later with hours of congestion and coughinglike their sinuses send an invoice at
bedtime.
For students and office workers, the biggest complaint is “I can’t focus.” Congestion and poor sleep make it harder to
pay attention, and frequent sneezing is basically the opposite of subtle. People who get the best control tend to use a
two-part approach: (1) a consistent nasal spray routine during the season, and (2) a fast-acting add-on (like an
antihistamine) on the days symptoms spike. The point isn’t to take everything all the timeit’s to match the tool to
the symptom pattern.
Eye symptoms have their own storyline. Some people can handle the sneezing, but itchy eyes drive them nutsespecially
if they wear contacts. Those who do well often keep a “mini kit”: antihistamine eye drops, a spare pair of glasses, and
a habit of washing hands before touching their face. It sounds basic, but when your eyes are itching, your brain will
try to convince you that rubbing them is a reasonable life choice. It’s not. It just spreads allergens and makes the
inflammation worse.
Then there’s the long-game experience: people who finally see an allergist after “toughing it out” for years. A common
reaction is regretnot because the visit was scary, but because they didn’t do it sooner. Once someone confirms ragweed
sensitivity with testing, they can make a targeted plan, and if needed, consider immunotherapy. Many describe
immunotherapy as the first time fall stopped feeling like an annual punishment. It’s not instant, and it takes
commitmentbut for the right person, it can be the difference between “surviving” autumn and actually enjoying it.
The biggest takeaway from real-life stories is simple: ragweed allergy is treatable, but it usually takes a plan.
People who feel best during ragweed season aren’t “lucky”they’re consistent. They start early, reduce exposure where
it’s easy, and use proven medications correctly. And they give themselves permission to treat allergies like the real
health issue they arenot a personal flaw.