Table of Contents >> Show >> Hide
- Why RA Medications Can Make Sunburn Worse
- Which Rheumatoid Arthritis Drugs May Increase Sunburn Risk?
- Signs You’re Having a Medication-Related Sun Reaction (Not Just “Regular Sunburn”)
- Sun Protection That Actually Works (Not Just “I Own Sunscreen”)
- What to Do If You Get Sunburned (or Think It’s Photosensitivity)
- Specific, Real-World Examples (Because Life Isn’t a Lab Study)
- How to Talk to Your Doctor or Pharmacist (Without Feeling Awkward)
- Extra: of Experiences Related to RA Drugs and Sunburn Risk
- Bottom Line
Rheumatoid arthritis (RA) is already a full-time job: joints that hurt for no good reason, fatigue that shows up uninvited, and a medicine schedule that can feel like running a tiny pharmacy out of your kitchen. So when someone says, “By the way, your RA drugs might make you burn faster in the sun,” it’s fair to respond with a long, dramatic sigh.
Here’s the good news: you don’t have to break up with summer. You just need a smarter relationship with sunlight. Some RA medications can increase photosensitivity, meaning your skin may react more strongly to ultraviolet (UV) lightsometimes with a sunburn-like reaction, sometimes with a rash, and sometimes with a “Why is my skin angry in exactly the shape of my T-shirt collar?” situation.
This article breaks down which rheumatoid arthritis drugs may increase sunburn risk, why it happens, what the reactions look like, and how to protect yourself without living life like a stylish indoor cat.
Why RA Medications Can Make Sunburn Worse
“Photosensitivity” is an umbrella term for skin reactions triggered when UV light interacts with a medication (or its byproducts) in or on your skin. Think of it like your medicine becoming a tiny hype person for UV raysexcept the hype is extremely unhelpful.
Two common types of drug-related sun reactions
- Phototoxic reactions: More common. They can look and feel like an exaggerated sunburnredness, burning, swelling, and sometimes blisteringoften on sun-exposed areas (face, neck, forearms, tops of feet).
- Photoallergic reactions: Less common. More like an eczema-style rash (itchy, bumpy, irritated), and it can appear latersometimes after you’ve already gone inside and congratulated yourself for “being careful.”
Beyond immediate discomfort, repeated UV damage matters long-term. Some medications (especially those that suppress the immune system) can also reduce your skin’s ability to repair UV damage over time, which is one reason clinicians emphasize sun protection for people taking certain immunosuppressive therapies.
Which Rheumatoid Arthritis Drugs May Increase Sunburn Risk?
Not every RA medication causes photosensitivity, and reactions vary widely from person to person. Two people can take the same drug and have totally different sun experiences: one gets a mild rash; the other becomes a human lobster after a “quick five minutes” outside.
The safest move is to check your prescription guide, ask your pharmacist, and pay attention to your own skin. But the medications below are commonly discussed in connection with sun sensitivity or sunburn-like reactions.
1) NSAIDs used for RA pain (especially certain types)
Nonsteroidal anti-inflammatory drugs (NSAIDs) are often used in RA to help manage pain and inflammation. Some NSAIDs are known to trigger photosensitivity in certain people. That doesn’t mean “never take them,” but it does mean “don’t assume your usual sun habits still apply.”
- Naproxen is frequently mentioned in photosensitivity discussions.
- Ketoprofen and piroxicam have also been associated with sun-sensitizing reactions.
Practical example: If you normally tolerate a 20-minute walk without sunscreen, but you start naproxen and suddenly your forearms sting and redden after 10 minutes, that’s a clue worth taking seriously.
2) Methotrexate (DMARD)
Methotrexate is a cornerstone DMARD for RA. It’s also linked in multiple references to sun-related skin reactions. Some patients experience a sunburn-like reaction or a rash after UV exposure. Another phenomenon sometimes described is “recall” reactions, where previously irritated or sunburned areas become inflamed again.
Translation: your skin may keep receipts. That sunburn you got last year? Methotrexate might remind your body about it at the worst possible timelike the first weekend you finally book a beach day.
3) Hydroxychloroquine (DMARD)
Hydroxychloroquine is widely used across inflammatory and autoimmune conditions, including RA in some situations. Reports on sun sensitivity are mixed: some sources list it among medications that can contribute to photosensitivity, while older research suggests clinically significant photosensitivity may be uncommon. The real-world takeaway is simple: if you notice new burning, redness, rash, or unusual irritation after sun exposure, don’t ignore itbring it up with your clinician.
Also worth noting: hydroxychloroquine is well known for potential eye-related side effects with long-term use, and bright light sensitivity can show up in some contexts. Sunglasses with UV protection aren’t just for looking cool; they’re practical.
4) Leflunomide (DMARD)
Leflunomide is another DMARD used for RA. It has been listed among medications associated with photosensitivity in patient-facing drug guidance, and there are case reports in the medical literature describing phototoxic reactions. These reactions aren’t guaranteed, but sun protection is a smart baseline.
5) Sulfasalazine (DMARD)
Sulfasalazine is used in RA and other inflammatory conditions. Patient medication information often includes photosensitivity warnings, advising people to avoid prolonged sun exposure and use protective clothing and sunscreen.
6) Azathioprine and other immunosuppressants (less common in RA today, but still relevant)
Azathioprine has been used for RA (though it’s not as common as methotrexate-based regimens today). It is recognized as an immunosuppressant and is discussed in medical references that cover adverse effects and monitoring needs. Immunosuppressive therapy can raise the stakes for UV protection because your immune system plays a role in surveilling and repairing UV-related cellular damage.
The key point: if a medication meaningfully affects immune function, your dermatologist and rheumatologist will often be extra enthusiastic about sun protection and skin checks.
What about biologics and JAK inhibitors?
Many biologics and targeted therapies don’t have “classic photosensitivity” as a headline side effect the way some NSAIDs and older DMARDs do. However, immune-modulating therapies may still be part of a bigger skin-safety conversation, including infection risk and, for some drugs, potential changes in skin cancer risk profiles. This is exactly why individualized advice matters: your specific medication, dose, health history, and skin type all change the math.
Signs You’re Having a Medication-Related Sun Reaction (Not Just “Regular Sunburn”)
A drug-related reaction can look like a standard sunburn, but a few clues can make you suspicious (in the medically responsible way):
- It happens fast (burning and redness after limited exposure).
- It’s unusually intense compared to your normal sun tolerance.
- It’s sharply limited to exposed areas (like a dramatic watch tan line, except painful).
- It includes blistering, swelling, or a rash that feels different from typical sunburn.
- It repeatsevery time you’re outdoors, the same problem shows up.
Important: if you develop widespread blistering, fever, chills, severe pain, facial swelling, or signs of infection (spreading redness, pus, worsening warmth), seek medical care promptly. People taking immunosuppressive drugs should be especially cautious about skin infections.
Sun Protection That Actually Works (Not Just “I Own Sunscreen”)
Sun safety is about layers. Not clothing layers only (though yes), but multiple strategies working together so you’re not relying on one heroic squirt of SPF to do all the heavy lifting.
Step 1: Treat sunscreen like a tool, not a vibe
- Go broad-spectrum to cover UVA and UVB.
- Use at least SPF 30 for most people; higher can be helpful if you burn easily or are on photosensitizing meds.
- Apply enough: most adults need roughly a shot-glass amount to cover exposed body skin.
- Reapply every two hours, and after swimming or sweating.
Step 2: Upgrade your wardrobe (yes, this is a medical recommendation)
- Wide-brimmed hat (your face, ears, and scalp will thank you).
- UV-blocking sunglasses (especially helpful if you have light sensitivity).
- Long sleeves or UPF clothing for reliable coverage that doesn’t rub off.
Step 3: Use the “shadow rule” and time your sun
UV tends to be strongest when the sun is highest. Seek shade during peak hours when possible, and remember that water, sand, and snow can reflect UV and increase exposure even when you feel cooler.
Step 4: Avoid tanning beds (seriouslyno negotiation)
Tanning beds are concentrated UV exposure. If you’re on medications that can trigger photosensitivity, a tanning bed is basically the “speedrun” mode for a bad skin day.
What to Do If You Get Sunburned (or Think It’s Photosensitivity)
First: don’t stop your RA medication on your own. Some RA therapies need careful tapering or replacement planning, and abruptly stopping can trigger flares. Instead, treat the reaction and contact your clinician for guidance.
At-home basics for mild reactions
- Get out of the sun immediately and cool the skin with cool (not ice-cold) compresses.
- Moisturize with fragrance-free lotion or aloe gel if tolerated.
- Hydratesunburn pulls fluid into the skin and can contribute to dehydration.
- Consider pain relief (ask your clinician/pharmacist what’s appropriate given your meds and health conditions).
Call a clinician urgently if:
- You have blistering over large areas.
- You develop fever, confusion, or severe weakness.
- The area looks infected or keeps worsening.
- You’re on significant immunosuppression and the burn is more than mild.
Specific, Real-World Examples (Because Life Isn’t a Lab Study)
The “Quick Errand” Trap
You run out for groceries. It’s cloudy. You skip sunscreen. Thirty minutes later, your forearms feel hot and stingymore than usual. Clouds don’t block all UV, and photosensitizing meds can lower your threshold. Keep a small sunscreen in your bag or car so “quick errands” don’t become “unexpected consequences.”
The “I’m Just Gardening” Situation
Gardening is wholesome, therapeutic, andplot twistoften done in direct sun at midday. If you’re on an NSAID like naproxen or a DMARD associated with photosensitivity, consider a wide-brim hat, UPF sleeves, and scheduled shade breaks. Your tomatoes will still grow even if you stop acting like a solar panel.
The “Vacation Sun Reflector” Surprise
Beach days feel breezy, but water and sand reflect UV. That means your sun exposure can be higher than it feels. For RA patients on sun-sensitizing meds, beach sunscreen should be a routine: apply before leaving, reapply on schedule, and pair with a rash guard or cover-up.
How to Talk to Your Doctor or Pharmacist (Without Feeling Awkward)
You don’t need a dramatic speech. Try:
- “Does any of my RA medication increase sun sensitivity or sunburn risk?”
- “If I get a rash or burn easily, should we adjust anything?”
- “Are there ingredients in my topical creams that make UV reactions worse?”
- “Should I schedule routine skin checks?”
If you’ve already had a reaction, be ready with details: what time you were outdoors, whether sunscreen was used, where the rash/burn appeared, how fast it started, and photos of the reaction (your phone camera is suddenly a healthcare tool).
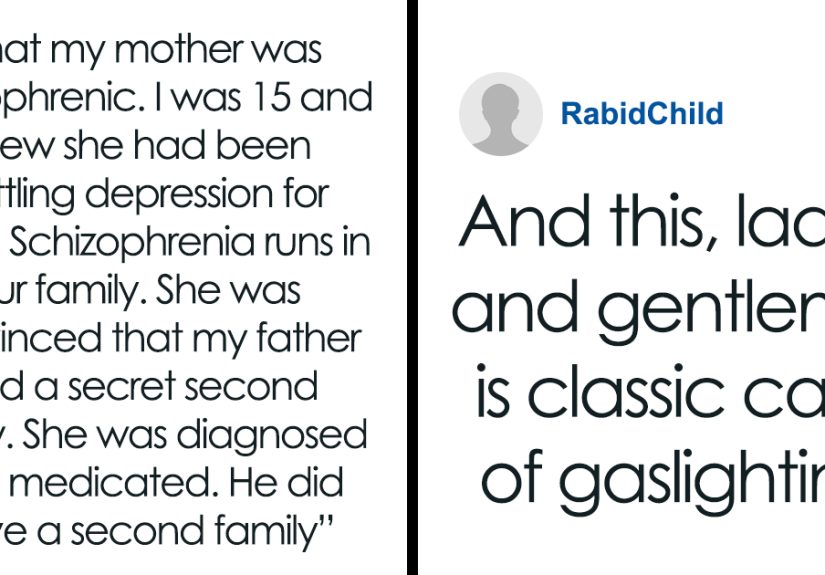
Extra: of Experiences Related to RA Drugs and Sunburn Risk
People’s experiences with RA medications and sun sensitivity often share a common theme: “I didn’t know that could happen… until it did.” The stories usually aren’t about someone spending eight hours sunbathing. They’re about normal lifewalking the dog, sitting at a kid’s soccer game, driving with sunlight hitting one arm through the windowand then noticing the skin reaction doesn’t match the amount of sun exposure.
One common experience goes like this: a person starts (or increases) an RA medication, feels better joint-wise, and becomes more active outdoors. They’re thrilledfinally moving again! Then they get a surprisingly painful burn after what felt like a modest amount of sunlight. The irony is brutal: the medication helps you reclaim your life, and the sun tries to invoice you for it.
Another frequently shared situation involves “mystery rashes.” Someone spends time outside, comes back in, and later develops an itchy, irritated rash on the chest, forearms, or hands. It doesn’t look like their usual sunburn, and it shows up late enough that it’s easy to blame laundry detergent, a new lotion, or even “something I ate.” When the pattern repeatssun exposure followed by the same rash in the same placesit starts to click that UV plus medication might be the real combo meal.
There are also experiences that highlight how specific and unfair photosensitivity can be. People describe having reactions in areas that were exposed for “just a little while,” like ankles between socks and pants, the back of the neck above a collar, or the tops of feet in sandals. It’s not only uncomfortableit’s confusing. These weird tan-line burns often push people to change habits: closed-toe shoes on bright days, a lightweight scarf for neck coverage, or simply committing to sunscreen as a daily routine rather than a beach-only accessory.
Some patients report that after a first strong reaction, they become much more consistent with protectionand the problem becomes manageable. They keep sunscreen in multiple places (bathroom, bag, car), choose clothing with reliable coverage, and plan outdoor time earlier or later in the day. The emotional shift matters too: instead of feeling like the medication “ruined” summer, they treat sun safety as another form of self-carelike stretching in the morning or taking meds on schedule.
The most helpful takeaway from these experiences is also the simplest: if your skin suddenly behaves differently in the sun after starting or changing RA medication, trust that signal. Bring it up with your care team. Often, you don’t need a dramatic medication changeyou just need a smarter sun strategy and clarity about what to watch for.
Bottom Line
Some rheumatoid arthritis drugs may increase sunburn risk or trigger sun-related rashes, especially certain NSAIDs and DMARDs. The solution usually isn’t avoiding the outdoorsit’s upgrading your protection plan. If you notice unusual burning, redness, blistering, or rashes after sun exposure, document it and discuss it with your doctor or pharmacist. Your RA treatment is meant to help you live more fully, not turn you into a vampire with great joints.