Table of Contents >> Show >> Hide
- The Mistake I Made: Confusing “Questions” With Evidence
- Why the Doctors Flagged RFK Jr. Specifically
- When Talking Points Become Policy: The Part I Didn’t Take Seriously Enough
- The Measles Reality Check: Nature Doesn’t Care About Our Discourse
- “Not Ruled Out” Is Not the Same Thing as “Proven”A Quick Science Refresher
- The Germany Episode: Misinformation Doesn’t Need a Passport
- The Ethics Problem: “Do Your Own Research” Meets “Do No Harm”
- What I’m Actually Apologizing For
- How to Stay Science-Based Without Turning Into a Robot
- Conclusion: The Plot Twist Was Listening to Professionals
- Extra: of Experience (a.k.a. How I Finally Learned This the Hard Way)
I owe several doctors an apology. Not the kind you toss out like a “sorry you feel that way” text, either. I mean a real apologyfull-bodied,
no artificial sweeteners, and with enough humility to make a podcast host uncomfortable.
For a while, I was that person. You know the one. The “I’m not saying he’s right, I’m just saying he’s asking questions” person. The “we need to
hear all sides” person. The “doctors shouldn’t be so dramatic” personspoken by someone who considers a 7-minute YouTube clip the equivalent of
a residency.
And the doctorsactual doctors, with the diplomas and the sleep deprivation to prove itkept saying the same thing:
“This isn’t harmless. When you mainstream medical misinformation, people get hurt.” I nodded like I was listening, then returned to my regularly
scheduled doomscrolling, convinced that “public health” was mostly a vibe and not, like… an entire discipline.
Reader, I was wrong. Spectacularly. Olympic-level wrong. And the part that stings isn’t just that I misjudged one public figure. It’s that I
underestimated the physics of bad information: once it’s moving, it doesn’t stop because you wish it would. It keeps goingthrough group chats,
school board meetings, clinics, and eventually policy.
The Mistake I Made: Confusing “Questions” With Evidence
Here’s how it happened. Someone would say: “RFK Jr. is dangerous on health policy.” And I’d respond with my favorite intellectual party trick:
“Isn’t it healthy to be skeptical?”
Skepticism is healthy. But skepticism is a method, not a personality. Real skepticism asks, “What would change my mind?” It collects data, weighs
the quality of evidence, and updates beliefs like a grown-up.
What I was doingwhat a lot of us dois something else. It’s the cosplay version of skepticism: asking questions that are designed to never be
answered, or treating every answer as suspicious by default. It’s “just asking questions” the way a toddler “just asks questions” when you say
the cookie jar is off-limits.
Doctors tried to tell me this. Public health folks tried too. They said: “There’s a difference between scrutinizing data and manufacturing doubt.”
I heard them. I just didn’t feel ituntil the doubt started showing up on official-looking letterheads.
Why the Doctors Flagged RFK Jr. Specifically
Let me be precise, because satire without facts is just yelling with punctuation.
The concern wasn’t that RFK Jr. had unpopular opinions. It was that he became one of the country’s most influential amplifiers of claims that
conflict with mainstream medical evidenceespecially around vaccinesoften framing settled questions as suspiciously unresolved, and portraying
health institutions as corrupt by default.
When clinicians warned me, they weren’t saying, “Disagree with us and you’re evil.” They were saying, “We’ve seen this movie: when people lose trust
in routine immunization and evidence-based guidance, preventable disease returns. And it doesn’t RSVP first.”
When Talking Points Become Policy: The Part I Didn’t Take Seriously Enough
This is where my denial really shineslike a beacon, but make it embarrassing.
I told myself: “Even if he says questionable things, the system has guardrails.” I imagined a kind of bureaucratic Roomba that bumps into a wall and
automatically turns toward science.
Here’s what I learned: guardrails matter, but who you put in charge of the steering wheel matters more.
Under RFK Jr.’s leadership at the U.S. Department of Health and Human Services, multiple vaccine-related policies and processes were reported as
shifting in ways that alarmed medical organizationsespecially when changes appeared to bypass the usual advisory pathways or reshape the groups that
inform recommendations. That’s not a minor administrative detail. It’s how “debate club” can quietly replace “evidence review.”
A big example: recommendations can change faster than the science
In an evidence-based world, recommendations change when new, high-quality data changes the balance of benefits and risks. In a politics-meets-public-health
world, recommendations can also change because the people in the room change, the questions change, and the standards of proof get rearranged like furniture
in a dark living room.
And when the public sees whiplashespecially around pregnancy, childhood schedules, and long-standing guidanceit doesn’t interpret it as a nuanced
update. It interprets it as: “They lied before” or “They’re guessing,” even when the reality is more complicated.
The Measles Reality Check: Nature Doesn’t Care About Our Discourse
Here’s the part doctors understood in their bones: viruses are not impressed by your personal brand.
Measles, in particular, is brutally efficient. It spreads easily, and controlling it depends on consistently high vaccination coverage.
Once coverage drops in pocketswhether because of access problems, misinformation, or rising exemptionsoutbreaks can ignite and travel.
When doctors warned that normalizing vaccine doubt could lead to preventable outbreaks, I treated it like a hypothetical. But outbreaks aren’t hypotheticals.
They’re receipts. And they arrive whether or not you’ve read them.
“Not Ruled Out” Is Not the Same Thing as “Proven”A Quick Science Refresher
One reason misinformation thrives is that it borrows the language of scienceespecially the cautious partsand uses it like a Halloween costume.
Science almost never says “never.” Science says “based on the best available evidence, here’s what’s likely, here’s what’s unlikely, and here’s what we
still don’t know.” That humility is a feature, not a bug.
But here’s the trick: if you treat “we can’t prove an absolute negative in every imaginable scenario” as “therefore anything is plausible,” you’ve
turned scientific caution into a conspiracy vending machine.
High-quality evidence looks like large, well-designed studies; converging results across different populations; biologically plausible mechanisms; and
transparent review by experts with relevant backgrounds. It also looks like willingness to say, “We checked. We don’t see an increased risk,” and to
update if better data appears.
Why doctors keep bringing up the autism-vaccine claim
Not because they enjoy arguing on the internet. Because it’s one of the most durable examples of how a scary claim can outlive the evidence against it.
The most responsible scientific reviews don’t treat every claim as equally supported. They evaluate strength. For example, major evidence reviews have
described epidemiologic findings showing no increased risk of autism associated with the MMR vaccine, with conclusions grounded in that body of research.
When you understand that, you also understand why clinicians lose patience when public figures keep “reopening” the same claim as if it’s breaking news.
That’s not curiosity. That’s rerunning an old movie and pretending it’s a documentary.
The Germany Episode: Misinformation Doesn’t Need a Passport
Another thing the doctors were right about: once you build an audience around suspicion, the claims don’t stay neatly contained.
They jump borders, contexts, and legal systems.
When public officials repeat sensational claims about other countriesespecially claims involving doctors, vaccines, and punishmentit can fuel fear and
deepen mistrust, even if the claim collapses under basic fact-checking.
I used to shrug and say, “People will figure it out.” Doctors kept saying, “No, people will share it. And then someone will skip care because they’re
scared.” Turns out, the doctors understood human behavior better than I did. (This is shocking only if you’ve never seen a waiting room.)
The Ethics Problem: “Do Your Own Research” Meets “Do No Harm”
I also owe doctors an apology for dismissing their ethical discomfort.
Medicine isn’t just about being technically correct. It’s about responsibilityespecially when you’re dealing with children, pregnancy, and population-level
prevention. That’s why clinicians and bioethicists get nervous when medical policy starts resembling a social media experiment.
If there’s controversy around research programs, advisory processes, or the way recommendations are rewritten, the ethical stakes aren’t abstract:
the consequences land on newborns, immunocompromised patients, and communities with less margin for error.
Here’s what I learned from watching how doctors talk about these issues: they don’t demand perfection. They demand integrityclear evidence standards,
relevant expertise at the table, transparency about uncertainty, and a bias toward protecting the most vulnerable.
What I’m Actually Apologizing For
I’m apologizing for the smugness. For treating medical consensus like it was an opinion column.
For assuming that because science evolves, it must be unreliablelike concluding that because weather changes, meteorologists are scammers.
I’m apologizing for confusing “distrust” with “discernment.” For acting like the loudest critic automatically deserves equal weight to the people
who spend decades studying immunology, epidemiology, maternal-fetal medicine, and infectious disease.
I’m apologizing for underestimating the downstream effectshow a few high-profile claims can become a thousand low-stakes decisions:
one delayed shot, one skipped appointment, one school exemption that feels private but adds up publicly.
How to Stay Science-Based Without Turning Into a Robot
The good news: you don’t have to choose between blind trust and permanent suspicion. There’s a middle pathcall it “adult skepticism.”
Here are a few habits I wish I’d adopted earlier:
1) Ask “What would convince me I’m wrong?”
If the answer is “nothing,” you’re not doing analysisyou’re doing identity.
2) Look for convergence, not viral certainty
One study is a clue. Multiple well-designed studies pointing the same directionacross countries, systems, and timestarts to look like reality.
3) Separate “possible” from “probable”
Many things are possible. The question is: what does the best evidence say is likely? Public health guidance is built on probability, not on the most
cinematic hypothetical.
4) Check who benefits from the doubt
Attention is a currency. So is outrage. If a claim spreads because it makes you feel special for “knowing the truth,” pause. That’s a marketing strategy,
not a peer review.
5) Use your clinician as a translator, not a punching bag
Your doctor isn’t offended by questions. They’re exhausted by recycled misinformation packaged as “concerns.” Bring the claim. Ask for context.
Let them do what they trained for: interpret evidence.
Conclusion: The Plot Twist Was Listening to Professionals
The doctors were rightnot because doctors are always right (they’ll be the first to tell you they aren’t), but because they were tracking something
I ignored: the difference between healthy debate and corrosive doubt.
I used to think the worst-case scenario of medical misinformation was awkward Thanksgiving conversation. Now I understand the real worst-case scenario:
preventable disease, policy chaos, and a public that stops trusting the very tools designed to keep it safe.
So yes. I owe several doctors an apology. And maybe a coffee. Possibly a nap. Definitely a promise:
next time, I’ll treat evidence like evidenceand stop confusing “loud” with “true.”
Extra: of Experience (a.k.a. How I Finally Learned This the Hard Way)
My shift didn’t happen all at once. It happened the way most adult learning happens: in small humiliations, inconvenient moments, and one extremely
sincere conversation that made it impossible to go back to my old certainty.
The first crack appeared in a pediatric waiting room. A parent near me was whisper-arguing with the receptionist about a vaccine form. Not yelling.
Not grandstanding. Just… anxious. The kind of anxiety that isn’t theatrical; it’s practical. The parent kept saying, “I read that this shot can cause
problems,” and the receptionist kept repeating, gently, that the clinician could go over it. The parent wasn’t trying to be difficult. They were trying
to be safeusing the tools the internet gave them, which is like trying to cook dinner with a flamethrower because someone said it “kills germs.”
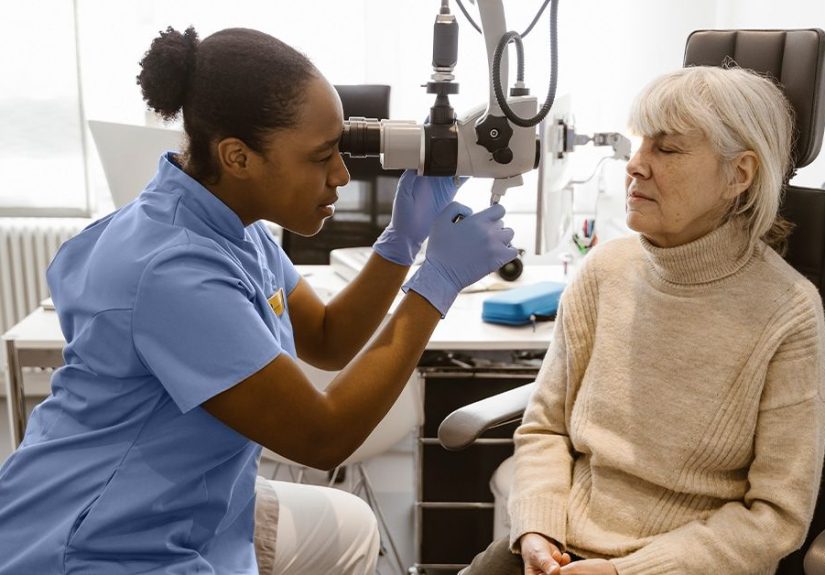
Then I watched the nurse come out and handle it. No eye-rolling. No “how dare you.” Just calm questions:
“What did you read?” “Where did it come from?” “What part worries you most?” She translated risk the way professionals doby comparing it to real risks,
not to vibes. She explained what the vaccine prevents, how common serious complications are, and what symptoms to watch for after any immunization.
The parent’s shoulders visibly dropped. Not because they were bullied, but because someone finally offered clarity instead of algorithms.
The second crack was a friend who was pregnant. She wasn’t political. She wasn’t trying to be edgy. She was just overwhelmed by contradictory headlines.
One day she said, “I don’t even know what I’m allowed to trust anymore,” and I realized my “all sides” posture didn’t help real people who needed real
decisions. Pregnancy is already a masterclass in unsolicited opinions. Adding policy whiplash to it is like juggling while someone keeps changing the
gravity settings.
The third crack was a school email about immunization documentation. It was boringbureaucratic evenand that’s why it hit me. Public health isn’t
mostly dramatic debates. It’s mostly systems: forms, schedules, reminders, checklists, and quiet prevention that nobody celebrates because nothing
terrible happened. When trust erodes, those boring systems become battlegrounds. And the casualties aren’t theoretical. They’re the kids who miss class,
the parents who miss work, the clinics that scramble, and the communities that discover too late that “personal choice” has group consequences.
Finally, I talked to a physician who looked more tired than my phone battery after a day of “research.” They said, “I don’t need everyone to agree with
me. I need people to stop treating public health like a prank call.” That sentence stuck. It wasn’t ideological. It was protective.
That’s when I understood what my earlier self refused to grasp: doctors weren’t being dramatic about RFK Jr. because they love institutions.
They were being dramatic because they love patients. And patients don’t get to opt out of reality.