Table of Contents >> Show >> Hide
- First: What Kind of Jaw Pain Are We Talking About?
- What Exactly Is a Dental Mouthguard (Night Guard/Occlusal Splint)?
- When a Mouthguard Can Help Jaw Pain
- When a Mouthguard Might Not Help (or Could Make Things Worse)
- Over-the-Counter vs Custom Mouthguards: What’s the Difference?
- Do Mouthguards Actually Work for TMJ Pain?
- Potential Downsides and Risks (Yes, Even for “Just a Guard”)
- A Simple Decision Framework: Should You Try One?
- How to Use and Care for a Night Guard (So It Helps Instead of Hurts)
- What Else Helps Jaw Pain (Because a Mouthguard Shouldn’t Be Your Only Plan)
- Bottom Line: Should You Use a Dental Mouthguard for Your Jaw Pain?
- Real-Life Experiences: What People Commonly Notice When Using a Mouthguard for Jaw Pain
- Experience #1: “My mornings stopped feeling like I boxed a wall in my sleep.”
- Experience #2: “The guard felt weird… until it didn’t.”
- Experience #3: “I tried an OTC guard and it made my jaw angrier.”
- Experience #4: “The guard helped… but the real game-changer was daytime clenching.”
- Experience #5: “I expected a miracle. I got ‘steady improvement.’”
Jaw pain can be a real mood-killer. You wake up, you yawn, and your face acts like it just got a surprise pop quiz. If you’ve been told “Maybe you need a mouthguard,” you’re not alone. Dental mouthguards (often called night guards or occlusal splints) are common for teeth grinding and jaw clenchingand they can help some people with jaw pain. But they’re not a magic bite-sized cure-all, and the “right” choice depends on what’s actually causing your pain.
This guide breaks down when a dental mouthguard for jaw pain makes sense, when it doesn’t, the pros/cons of over-the-counter vs custom options, and how to avoid turning a helpful tool into an expensive chew toy.
Quick note: This is educational information, not personal medical advice. If your pain is severe, worsening, or tied to swelling, fever, recent injury, or trouble opening your mouth, get evaluated promptly.
First: What Kind of Jaw Pain Are We Talking About?
“Jaw pain” is a big umbrella. Under it you’ll find everything from tight muscles to joint inflammation to tooth problems pretending to be jaw problems. Many cases fall under temporomandibular disorders (TMD)issues involving the jaw joint (TMJ), jaw muscles, and surrounding structures. Symptoms can include:
- Aching jaw or facial pain
- Clicking/popping (sometimes painless and harmless)
- Morning soreness or headaches
- Pain when chewing
- Limited opening or “stuck” jaw
- Ear-area discomfort (the TMJ sits close to the ear)
And then there’s the sneaky culprit: bruxismteeth grinding or clenching during sleep or while awake. Some people clench like they’re trying to turn coal into diamonds. Bruxism can overload jaw muscles and irritate the joint, leaving you sore in the morning or after stressful days.
Red flags that shouldn’t wait for a mouthguard experiment
Call a dentist or medical professional soon (urgent if severe) if you have: facial swelling, fever, signs of infection, recent trauma, numbness, sudden bite change, severe tooth pain, or you can barely open your mouth. Mouthguards are for mechanical stressnot for infections, fractures, or serious joint conditions.
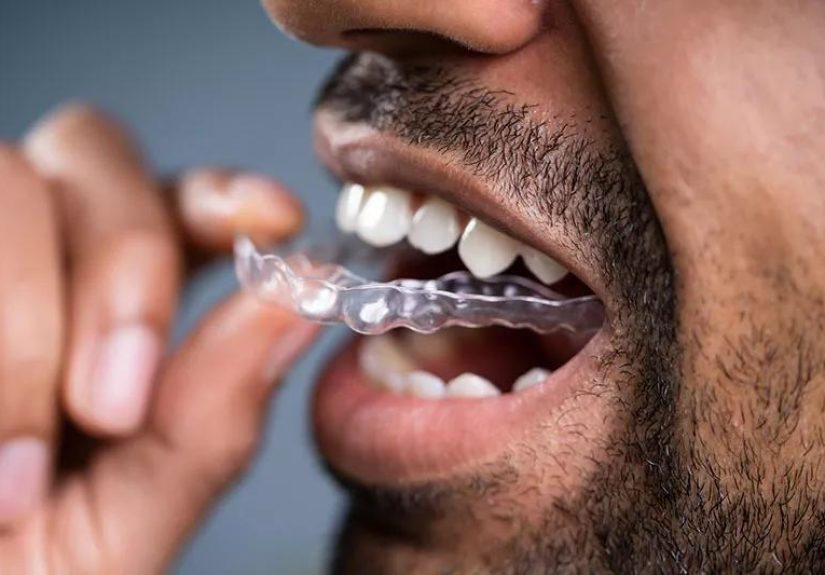
What Exactly Is a Dental Mouthguard (Night Guard/Occlusal Splint)?
A dental mouthguard for jaw pain is usually an appliance worn over your upper or lower teeth. It creates a barrier between teeth and can change how the teeth contact. Depending on the design, it may:
- Protect teeth from wear, chips, or cracks caused by grinding
- Reduce muscle overload by “smoothing out” how forces distribute
- Decrease joint stress in some cases
- Interrupt clenching patterns for certain people (especially with daytime awareness)
Important: a night guard is not the same thing as a sports mouthguard. Sports guards are built for impact protection. Night guards are built for bite forces and fit precision. Wearing the wrong type can feel like sleeping with a hockey puck.
Common types you’ll hear about
- Soft night guards: cushier, sometimes helpful for mild grinding, but can increase chewing/clenching in some people.
- Hard (acrylic) stabilization splints: firmer, often used for moderate/severe bruxism and some TMD patterns.
- Dual-laminate guards: soft inside, hard outsidecomfort plus durability.
- Repositioning splints: designed to change jaw position. These should be used only under close professional guidance because long-term use can affect the bite.
- Anterior bite appliances: cover only some teeth; can be useful in specific cases but are not “one-size-fits-all.”
When a Mouthguard Can Help Jaw Pain
A mouthguard is most likely to help when your jaw pain is strongly linked to clenching/grinding or muscle overuse. Here are situations where it often makes sense:
1) You have signs of grinding or clenching
Clues include flattened or worn teeth, tiny cracks, sensitive teeth without a clear cavity, a partner hearing grinding at night, or waking with jaw fatigue. In these cases, a night guard may not “cure” bruxismbut it can reduce damage and sometimes ease muscle soreness by changing the loading pattern.
2) Your pain is worst in the morning
Morning pain often points to nighttime clenching/grinding. A guard can act like a shock absorber and a protective barrier while you sleep.
3) You get tension headaches with jaw tightness
Overworked jaw muscles can contribute to temple headaches. A mouthguard can be part of a broader plan that includes stress management, jaw relaxation habits, and physical therapy-style exercises.
4) Your dentist suspects a “muscle-driven” TMD pattern
TMD is not one condition. If your exam suggests muscle tenderness and overactivity (rather than primarily joint degeneration), a stabilization-type guard is often considered a conservative optionespecially alongside home care.
Real-world example: A high school student starts waking up with jaw soreness during exam season. Their teeth show new wear facets and they catch themselves clenching while gaming. A custom night guard plus daytime “lips together, teeth apart” reminders and stress breaks can reduce morning pain over a few weeks. Not dramatic. Just… noticeably better. Like switching from running in dress shoes to sneakers.
When a Mouthguard Might Not Help (or Could Make Things Worse)
Mouthguards are helpful tools, but they’re not universal fixes. You’ll want caution if:
1) Your pain is mainly joint inflammation or arthritis
Some joint problems need targeted management beyond a guardlike anti-inflammatory strategies, guided therapy, or specialist evaluation. A guard can still be part of the plan, but it may not be the star player.
2) Your jaw locks, shifts, or you have significant limited opening
Locking and significant movement issues can signal internal joint problems. An appliance might be used, but the type and schedule matter. This is “professional supervision required” territory.
3) An over-the-counter guard fits poorly
A bad fit can irritate gums, create uneven pressure, and potentially worsen symptoms. If you try OTC and your pain increases, stop and get guidance.
4) The appliance is designed to permanently change your bite
Most major health authorities emphasize starting with conservative care and avoiding irreversible bite changes early on. A mouthguard should not be a stealth orthodontics project unless that’s clearly part of a carefully managed treatment plan.
Over-the-Counter vs Custom Mouthguards: What’s the Difference?
There are three broad categories:
Stock (pre-formed) guards
Cheapest, least fitted. Often bulky and can be uncomfortable. Generally not ideal for jaw pain management.
Boil-and-bite guards
You soften the material and mold it at home. They can be a reasonable short-term trial for some mild grinders, but the fit is usually less precise than a dentist-made device. If you have braces, significant dental work, or jaw pain that’s already intense, skip DIY molding and get professional input.
Custom night guards from a dentist
Made from impressions or digital scans of your teeth. The fit is typically better, comfort is higher, and the design can be matched to your needs (soft vs hard vs hybrid). Custom guards cost more, but they also tend to last longer and reduce the “this feels weird so I stop wearing it” problem.
Practical take: If your jaw pain is mild and you strongly suspect clenching, a carefully chosen boil-and-bite can be a short trial. If pain is moderate/severe, persistent, or you’ve had jaw locking, bite changes, or complex dental work, a dental evaluation and custom plan is the safer route.
Do Mouthguards Actually Work for TMJ Pain?
Here’s the honest answer: sometimesand the evidence is mixed depending on the exact diagnosis and the type of appliance. Many reputable resources note that oral splints may help some people with TMD pain, but results vary and the “why” isn’t always clear.
That doesn’t mean they’re useless. It means they’re best viewed as a conservative tooloften tried alongside self-care and habit changesrather than a guaranteed cure.
Think of a mouthguard like supportive shoes. The shoes can reduce strain, but they won’t fix a broken ankle. You still need the right diagnosis.
Potential Downsides and Risks (Yes, Even for “Just a Guard”)
- Initial discomfort: Some people feel extra salivation or dryness at first. This often improves with time.
- Soreness or worse pain: A poor fit, wrong design, or wrong wearing schedule can aggravate symptoms.
- Bite changes: Prolonged or inappropriate appliance use can sometimes change how teeth meetespecially with repositioning-type devices.
- Gum irritation: Rough edges or pressure points can irritate soft tissue.
- Hygiene issues: Guards can collect bacteria if not cleaned properly, which is not the kind of “biofilm” anyone wants.
Rule of thumb: If the mouthguard causes new pain, tooth tenderness, or a bite that feels “off” after you remove it, pause and talk with your dentist.
A Simple Decision Framework: Should You Try One?
You’re a good candidate to discuss a mouthguard if:
- You wake up with jaw soreness, tightness, or headaches
- You have signs of bruxism (worn teeth, chips, partner hears grinding)
- You catch yourself clenching during the day
- Your dentist notes muscle tenderness or bite-force wear
You should get evaluated first (and not DIY it) if:
- Your jaw locks, shifts, or opening is limited
- You have swelling, fever, or suspected infection
- You recently had facial/jaw trauma
- You have significant dental restorations, implants, or braces
- Your pain is severe or getting worse
Questions to ask your dentist (to avoid the “random plastic” approach)
- Do you think my pain is more muscle-related or joint-related?
- What type of guard do you recommend (soft, hard, dual-laminate), and why?
- How many hours should I wear itnight only or sometimes daytime too?
- What should I watch for that means it’s not working (or making things worse)?
- How often should we re-check the fit?
How to Use and Care for a Night Guard (So It Helps Instead of Hurts)
Wearing tips
- Follow the schedule: Most are nighttime-only unless your dentist instructs otherwise.
- Give it an adjustment window: Many people need a week or two to get used to the feel.
- Don’t chew on it: Your mouth is not a dog with a squeaky toy. Chewing can worsen clenching patterns and destroy the appliance.
Cleaning basics
- Rinse after use with cool or lukewarm water.
- Brush gently with a soft toothbrush (many dentists recommend mild soap; some toothpastes are too abrasive).
- Let it dry before storing to reduce bacterial growth.
- Keep it in a ventilated case away from heat (hot water can warp some materials).
Replacement timing: If it cracks, warps, gets rough edges, or no longer fits snugly, it’s time to be replaced or adjusted.
What Else Helps Jaw Pain (Because a Mouthguard Shouldn’t Be Your Only Plan)
Most professional guidance emphasizes conservative, reversible strategies first. The mouthguard often works best when paired with:
Jaw-friendly habits
- Keep lips together, teeth apart (your jaw muscles relax when teeth aren’t touching).
- Avoid gum chewing, nail biting, and “testing” your jaw by clicking it on purpose.
- Eat softer foods during flare-ups (think: scrambled eggs, yogurt, soupnot beef jerky).
Heat/ice and gentle movement
Moist heat can relax tight muscles; ice can calm inflammation. Gentle jaw stretches and controlled movement exercises (often taught by a clinician or physical therapist) can improve function over time.
Stress and sleep support
Stress is gasoline for clenching. Relaxation techniques, breathing drills, and better sleep routines can reduce triggers. If bruxism is severe, evaluation for sleep issues (including sleep apnea) may be relevant.
Medication (when appropriate)
Over-the-counter anti-inflammatories may help short-term for some people, if safe for you medically. For persistent cases, clinicians may consider muscle relaxants or other approaches based on the diagnosis.
Bottom Line: Should You Use a Dental Mouthguard for Your Jaw Pain?
If your jaw pain is linked to teeth grinding or jaw clenching, a dental mouthguardespecially a well-fitted night guardcan be a smart, conservative option to protect your teeth and potentially reduce muscle-related soreness. If your pain is driven by joint problems, inflammation, or something unrelated to bruxism, a mouthguard alone may do littleor even worsen symptoms if the fit/design is wrong.
The best move: Use a mouthguard as part of a broader plan: confirm the likely cause of your pain, pick the right type of appliance, monitor symptoms, and combine it with habit changes and self-care.
Real-Life Experiences: What People Commonly Notice When Using a Mouthguard for Jaw Pain
Because jaw pain is so personal (and so annoying), people tend to remember exactly what changed when they started wearing a night guard. Here are a few common experiences dentists and patients often describepresented as realistic composites, not individual medical stories.
Experience #1: “My mornings stopped feeling like I boxed a wall in my sleep.”
A lot of people don’t realize they’re clenching until they notice the pattern: sore jaw in the morning, tension headache by lunchtime, and a weird feeling that their teeth were “working overnight.” After starting a night guard, the first improvement is often less morning muscle fatigue. Not always instant, but noticeablelike someone turned the volume down on the ache. The biggest surprise? The guard doesn’t always stop clenching. Instead, it can make clenching less destructive and less painful.
Experience #2: “The guard felt weird… until it didn’t.”
The adjustment phase is real. People commonly report extra saliva, dryness, or the sensation that their mouth is “busy” for the first several nights. Some describe it as “sleeping with a tiny spaceship in my mouth.” After a week or two, many adaptespecially with a custom-fit guard. The key is that the guard should feel snug and stable, not like it’s auditioning for a role in a slapstick comedy by sliding around at 2 a.m.
Experience #3: “I tried an OTC guard and it made my jaw angrier.”
This happens more than people expect. A boil-and-bite guard can be okay for a mild grinder, but if the fit is bulky or uneven, it may create new pressure points. Some people notice their bite feels “off” in the morning or their jaw soreness increases. When that happens, the best experience is the one where they stop using it quickly and schedule a dental check rather than powering through pain. A mouthguard should not be a bravery test.
Experience #4: “The guard helped… but the real game-changer was daytime clenching.”
Many people discover that nighttime grinding is only half the story. They also clench while concentratingstudying, gaming, driving, scrolling, lifting weights, or dealing with stressful conversations. Once they start wearing a night guard, they become more aware of daytime clenching and add simple habits: jaw relaxed, teeth apart, tongue resting gently on the palate. Pairing a guard with these changes often leads to better results than the guard alone. It’s like realizing your phone battery problem isn’t the chargerit’s the 37 apps running in the background.
Experience #5: “I expected a miracle. I got ‘steady improvement.’”
For many, the most realistic outcome is gradual. Pain intensity decreases, flare-ups become less frequent, and chewing feels easier. But the guard doesn’t necessarily fix everythingespecially if the jaw pain is driven by joint inflammation, poor posture, or stress. People who do best tend to treat the mouthguard as one piece of a plan: they use heat/ice during flare-ups, avoid gum chewing, choose softer foods temporarily, and follow up for adjustments. Over time, that combination can turn jaw pain from a daily headline into an occasional footnote.
If you want your experience to land in the “steady improvement” category, focus on two things: proper fit and proper diagnosis. That’s the difference between a helpful guard and a fancy piece of plastic that lives in your bedside drawer forever.






