Table of Contents >> Show >> Hide
- What is a traumatic cataract?
- Causes of traumatic cataracts
- Symptoms of a traumatic cataract
- When to seek urgent care after an eye injury
- How doctors diagnose traumatic cataracts
- Treatment: what actually helps?
- Recovery: what to expect after treatment
- Possible complications and why follow-up matters
- Prevention: the easiest cataract to treat is the one you never get
- Quick FAQ
- Experiences: what living through a traumatic cataract can feel like (real-world stories, minus the drama soundtrack)
- The “Wait…why is everything hazy?” phase
- The “It’s only one eye, so I’ll be fine” phase
- The appointment that makes it real
- The decision about surgery (a.k.a. “How bad is bad enough?”)
- Surgery day and the surprisingly unglamorous heroism of eye drops
- The “OhTHAT’S what colors look like” moment
- What people wish they’d known sooner
The word “cataract” usually shows up in conversations about agingalongside other classics like “my knees predict rain.”
But a traumatic cataract is the plot twist: the lens inside your eye turns cloudy after an eye injury,
and it can happen to people who are nowhere near “retirement age.”
This article breaks down what a traumatic cataract is, what causes it, what symptoms to watch for, and how it’s treatedplus
practical prevention tips (because your eyes are not replaceable parts from a hardware store).
What is a traumatic cataract?
A traumatic cataract is a clouding of the eye’s natural lens that occurs after an injury. The lens is normally clear and helps focus light
so you can see sharply. Trauma can disrupt the lens fibers, damage the lens capsule (the “wrapper” around the lens), or trigger inflammation that leads
to gradual clouding over time.
Unlike many age-related cataracts that creep in slowly, traumatic cataracts can appear quickly (sometimes soon after an injury) or
show up months or even years later. That delayed timing is one reason people sometimes don’t connect today’s blurry vision with that
“I walked into a cabinet door” moment from long ago.
Causes of traumatic cataracts
Traumatic cataracts can result from several types of eye trauma. The common theme: something disrupts the lens structure or its protective capsule.
1) Blunt eye trauma
Blunt trauma means the eye was struck without something piercing itthink sports injuries, a fall, an elbow during a pickup game, a car accident with
impact forces, or a work-related accident. Blunt force can compress and stretch the eye, stressing the lens fibers and their support structures
(the zonules). A classic finding after blunt injury is a rosette- or flower-shaped lens opacity, often called a “rosette cataract.”
2) Penetrating or perforating injury
If a sharp object enters the eye, it can directly damage the lens capsule. When the capsule is disrupted, lens proteins and fluid changes can cloud the lens
faster. Penetrating injuries are also more likely to involve other structures, which can make treatment more complicated.
3) Chemical, radiation, or electrical injury
Less common, but still real: chemical exposure, certain types of radiation exposure, or electrical injury can contribute to lens damage and cataract development.
These scenarios are more likely to come up in workplace or medical-treatment contexts.
4) “Why now?”Delayed traumatic cataracts
A traumatic cataract can be immediate, but it can also be delayed. Some injuries cause subtle lens damage that becomes more obvious over time. In other cases,
the injury triggers inflammatory changes that slowly affect lens clarity. The result: a cataract that seems to arrive “out of nowhere,” but actually had a
long runway.
Symptoms of a traumatic cataract
Traumatic cataracts often cause the same visual symptoms as other cataracts, but they may be one-sided (affecting just the injured eye)
and may show up sooner than you’d expect.
- Blurry, cloudy, foggy, or “film-over-the-eye” vision
- Glare and light sensitivity (headlights, bright sun, lamps)
- Seeing halos around lights
- Trouble seeing at night or in low-contrast situations
- Colors that look faded or less vivid
- Double vision in one eye (monocular double vision)
- Needing brighter light to read or do close-up work
Important note: not every post-injury vision problem is a cataract. Trauma can also affect the cornea, iris, retina, optic nerve, or eye pressure.
That’s why a proper exam matterseven if your symptoms sound “cataract-y.”
When to seek urgent care after an eye injury
If the injury is recent and your vision changes suddenly, treat it like an emergency. Go to an emergency department or urgent eye clinic right away if you have:
- Sudden, significant vision loss or rapidly worsening vision
- Severe eye pain or intense light sensitivity
- Visible eye deformity or a markedly irregular pupil
- History that suggests a high-risk injury (for example, high-velocity metal-on-metal work)
If a serious injury is suspected, avoid pressing on the eye. In emergency settings, clinicians may use a protective shield rather than a pressure patch
to avoid squeezing the eyeball.
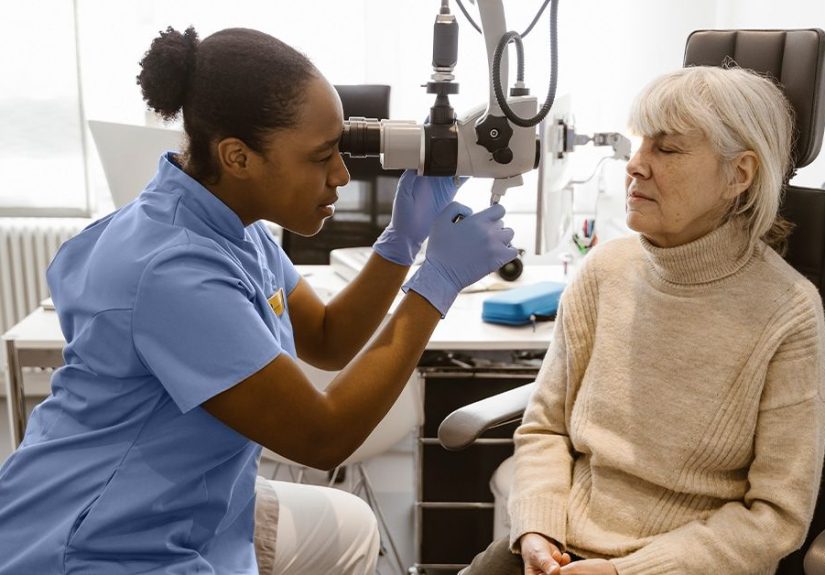
How doctors diagnose traumatic cataracts
Diagnosis typically starts with a comprehensive eye exam. Your clinician may check:
- Visual acuity (how clearly you see at different distances)
- Pupil response and a general assessment for signs of significant injury
- Slit-lamp exam to look at the lens, capsule, cornea, and anterior chamber
- Dilated eye exam to examine the retina and optic nerve (if safe to do so)
If the view to the back of the eye is blocked or a foreign body is suspected, imaging may be used. In many emergency protocols,
CT imaging is preferred to evaluate for certain traumatic findings and foreign bodies, especially when metal is involved.
Treatment: what actually helps?
The right treatment depends on two big things: (1) how much the cataract affects vision and (2) what else was injured.
Traumatic cataracts can be trickier than typical cataracts because trauma may also damage the capsule, zonules, iris, or other structures.
Step 1: Address the injury first
If the cataract developed after a recent injury, the first priority is to rule out and treat any urgent eye damage. That may include controlling inflammation,
managing eye pressure, treating associated injuries, and coordinating specialty care.
Step 2: Non-surgical options (when symptoms are mild)
Cataracts don’t dissolve with eye drops, vitamins, or wishful thinking. But if the cataract is small or not yet disrupting daily life, clinicians may recommend:
- Updating glasses or contact lenses
- Brighter lighting for reading and close tasks
- Anti-glare sunglasses or lenses
- Magnifying lenses for detailed work
These strategies can buy timebut they don’t remove the cataract. If vision loss interferes with daily activities, surgery is usually the definitive option.
Step 3: Surgery (the main event)
Cataract surgery removes the clouded lens and typically replaces it with an intraocular lens (IOL).
In routine cases, this is one of the most common surgeries performed in the U.S.but traumatic cataract surgery can be more complex because surgeons may need
to manage capsule tears, zonular weakness, adhesions (synechiae), bleeding, or other trauma-related changes.
Timing: should surgery happen right away?
There isn’t a one-size-fits-all schedule. Some traumatic cataracts can be observed until inflammation quiets down. Others need earlier interventionespecially if
the cataract is rapidly worsening, the capsule is disrupted, the lens is swelling, or vision loss is severe. Your ophthalmologist weighs surgical risk against
visual benefit and the condition of other eye structures.
How surgeons plan a traumatic cataract procedure
Traumatic cataract surgery often involves extra planning. Examples of considerations include:
- Capsule integrity: if the lens turns opaque quickly after injury, surgeons may suspect a capsule tear and adjust technique to avoid worsening it.
- Zonular damage: if the lens support is weak, surgeons may use specialized devices (like hooks or tension rings) to stabilize the capsular bag.
- Iris issues and inflammation: prior inflammation can create adhesions that reduce dilation, requiring careful management during surgery.
- IOL selection/placement: if the capsular bag is intact, the IOL can often be placed “in the bag.” If support is compromised, other fixation methods may be needed.
Pediatric traumatic cataracts: a special case
When children develop a traumatic cataract, timing and treatment decisions can be more urgent. Kids’ visual systems are still developing, and even small central
lens opacities can interfere with vision development and increase the risk of amblyopia (“lazy eye”). Because of that, clinicians may have a lower
threshold to treat visually significant cataracts in children and pair surgery with amblyopia management (like patching therapy) when needed.
Recovery: what to expect after treatment
Recovery varies depending on the severity of the injury and the complexity of surgery. After cataract surgery, many patients use a course of prescription eye drops
(often antibiotic and anti-inflammatory) and attend follow-up visits (commonly day 1, week 1, and around a monththough schedules vary).
Vision improvement can be noticeable quickly, but your eye may need time to fully settle. If the trauma also affected the retina, cornea, or optic nerve, vision may
improve only partiallyso the goal may be “best possible vision” rather than “back to 4K.”
Possible complications and why follow-up matters
Cataract surgery is generally safe, but traumatic cataract cases can carry additional risks because the injury may have weakened the eye’s internal support structures.
Potential issues your ophthalmologist may watch for include:
- Inflammation that needs longer treatment
- Changes in eye pressure (sometimes requiring pressure-lowering drops)
- Vitreous prolapse or the need for vitrectomy in more complex cases
- Other trauma-related complications depending on which eye structures were affected
The good news: careful planning, modern surgical tools, and good follow-up care can make outcomes very strongespecially when the rest of the eye is healthy.
Prevention: the easiest cataract to treat is the one you never get
A lot of traumatic cataracts start with preventable injuries. Eye protection isn’t glamorous, but neither is explaining to your boss that you got taken out by a
rogue wood chip.
- Wear protective eyewear for work hazards (construction, yardwork, lab work, power tools)
- Use sport-appropriate eye protection for high-risk activities
- Supervise kids around projectiles and high-velocity toys
- Keep safety gear comfortable and properly fitted so you’ll actually wear it
Quick FAQ
Can a traumatic cataract go away on its own?
Cataracts generally don’t “clear up.” Some symptoms may fluctuate with lighting or inflammation, but the clouding itself typically does not reverse.
If the cataract becomes visually significant, surgery is usually the effective treatment.
Is traumatic cataract always an emergency?
The cataract itself might not be an emergency, but the injury that caused it can be. If trauma is recentespecially with sudden vision change,
severe pain, or concern for penetrating injuryseek urgent evaluation.
Will cataract surgery restore perfect vision?
Many people see major improvement, but final vision depends on whether other parts of the eye were damaged by trauma. Your ophthalmologist can give a more specific
prognosis after a full exam.
Experiences: what living through a traumatic cataract can feel like (real-world stories, minus the drama soundtrack)
Medical explanations are helpful, but lived experience is often what people really want to know: “What does this feel like day-to-day?” Below are common
experiences people report during the traumatic cataract journey. Think of these as realistic compositesnot a promise that your exact path will match, but a map of
what many patients recognize.
The “Wait…why is everything hazy?” phase
A lot of people notice the change in ordinary moments: streetlights look like they’re wearing fuzzy halos, reading feels harder even with glasses, or one eye
seems like it has a permanent smudge on the “camera lens.” If the trauma happened recently, the frustration is sharper: you remember exactly what your vision was
like before. If the trauma was years ago, it’s more confusingyour brain starts bargaining: “Maybe I just need more sleep.”
The “It’s only one eye, so I’ll be fine” phase
When a traumatic cataract affects one eye, people often adapt without realizing it. The brain leans on the better eye, and you develop quiet workarounds:
turning your head slightly, avoiding night driving, or sitting in the “good angle” at a meeting. The downside is that depth perception can feel off, and fatigue
creeps in because your visual system is working overtime.
The appointment that makes it real
Hearing “traumatic cataract” can be oddly validatingfinally, a name for what you’re seeingbut it also raises a million questions in five seconds:
“Is it permanent? Is it dangerous? Do I need surgery? Did I do something wrong?” Good clinicians slow the moment down: they explain what’s cloudy, whether other
structures were affected, and what the next step is. Patients often say the biggest relief is learning there’s a plan.
The decision about surgery (a.k.a. “How bad is bad enough?”)
Many people don’t choose surgery because they “want perfect vision.” They choose it because normal life starts shrinking. Night driving becomes stressful.
Screens feel harsher. Sports get sketchy. Work takes longer. Parents notice their child turning an eye, squinting, or struggling with schoolwork. The tipping
point is usually practical: “I can’t do what I need to do anymore.”
Surgery day and the surprisingly unglamorous heroism of eye drops
People often describe cataract surgery as emotionally bigger than physically painful. The procedure itself is typically quick, but the meaning of it hits hard:
you’re trusting someone to work on your vision. Afterward, the recovery routine becomes the main characterdrops on schedule, follow-up visits, avoiding rubbing,
and being a little extra careful. If there was trauma-related complexity, follow-up can feel more frequent, and patience becomes part of the prescription.
The “OhTHAT’S what colors look like” moment
When recovery goes well, patients often describe a moment where the world looks cleanerlike someone wiped a foggy window. Whites look whiter. Contrast returns.
Text sharpens. And yes, some people genuinely say, “I didn’t realize how dim everything had become.” If the injury also affected other parts of the eye, the
improvement may be partialbut even partial improvement can mean getting back to work, hobbies, and confidence.
What people wish they’d known sooner
- Eye protection is not optional when the task has riskpeople regret skipping it for “just one quick thing.”
- Symptoms don’t always show up right away, so mention old injuries during eye exams even if they feel irrelevant.
- Recovery is a process, not a single “fixed” momentespecially after trauma.
- Emotions are normal: anxiety, impatience, relief, and gratitude can all show up in the same week.
If you’re reading this while dealing with an eye injury or changing vision, the best next step is simple: get evaluated by an eye care professional. Vision problems
after trauma are too important to “wait and see” in the casual sensesave that phrase for movie sequels, not eyeballs.