Table of Contents >> Show >> Hide
- Surrogate Partner Therapy in plain English
- Is it sex work? Why people get confused
- Who might consider surrogate partner therapy?
- How the triadic model actually works
- What happens in sessions?
- Training, professionalism, and ethics
- Is surrogate partner therapy legal in the U.S.?
- What does the research say? (Spoiler: more would be nice)
- Benefits people often report
- Risks and concerns (the grown-up section)
- How to find surrogate partner therapy the safer way
- Frequently asked questions
- Bottom line
- Real-World Experiences: What it can feel like (500-word add-on)
- SEO tags (JSON)
If “surrogate partner therapy” sounds like something you’d only hear whispered in a movie theater lobby (right next to “I swear the book was better”), you’re not alone.
It’s a real, structured modality used in sex therapyoften misunderstood, frequently sensationalized, and occasionally confused with things it’s not.
Surrogate Partner Therapy (SPT) is a form of experiential therapy where a client works with a licensed therapist and a trained surrogate partner in a
three-person therapeutic teamoften called a triadic model. The therapist guides the overall treatment plan, the surrogate partner works
directly with the client through practical, step-by-step experiences, and the client processes, practices, and integrates what they learn across both relationships.
The goal is not “hooking up with homework.” The goal is building skills: comfort with closeness, communication, boundaries, touch, sexual confidence,
emotional regulation, and (for some clients) the ability to experience intimacy without fear running the entire show.
Surrogate Partner Therapy in plain English
Some challenges can be talked through beautifullyand some can’t be fully resolved with talk alone. If a person’s struggles center on physical intimacy (touch anxiety,
shame, panic, dissociation, shutdown, performance fears, difficulty receiving affection), it can help to practice in real time with a trained professional.
That’s where surrogate partner work comes in.
In SPT, the surrogate partner may guide structured exercises that build from lower-intensity skills (breathing, eye contact, communication practice) toward
progressively more intimate experiences (non-sexual touch, sensual touch, clothed or unclothed body awareness, andin some casessexual contact). The pace is
individualized, consent-based, and intentionally gradual.
Is it sex work? Why people get confused
Let’s address the confusion directly, because the internet will not do it for us.
What SPT is
- Therapeutic: It’s part of a clinical treatment plan overseen by a therapist.
- Collaborative: The therapist and surrogate partner coordinate (with the client’s consent) to support agreed-upon goals.
- Skill-building: The focus is on learningcommunication, boundaries, nervous-system regulation, intimacy competence.
- Time-limited: Work is typically goal-based and ends when targets are met or the therapeutic arc is complete.
What SPT is not
- Dating: Feelings can arise because humans are human, but the relationship has therapeutic boundaries and a planned ending.
- A loophole: It is not designed to “sneak around” laws or ethics.
- Automatic intercourse: Sexual activity is not guaranteed, and many clients never go there. The work often focuses on intimacy without intercourse.
The key difference is the therapeutic container: treatment goals, informed consent, coordination with a supervising therapist, and structured progression.
If any of that is missing, you’re not looking at surrogate partner therapyyou’re looking at something else (and it might not be safe or ethical).
Who might consider surrogate partner therapy?
SPT isn’t a first stop. Most people begin with a licensed therapist (often a certified sex therapist) and explore SPT only if talk therapy alone isn’t enough to
create change in real-world intimacy.
Common reasons people explore SPT include:
- Severe sexual anxiety or panic around touch, nudity, arousal, or sexual performance
- Intimacy avoidance rooted in shame, strict upbringing, or chronic fear of rejection
- Trauma-related barriers (when the client and therapist agree experiential work is appropriate and trauma-informed safeguards are in place)
- Disability or medical history that complicates dating, sexual confidence, or physical intimacy
- Inexperience that fuels intense self-consciousness or “I missed the memo everyone else got at 16” distress
- Body image distress that makes being seen, touched, or desired feel unbearable
- Difficulty with boundaries (either too rigid or too porous), especially in romantic or sexual situations
Importantly, SPT is not a “quick fix” for loneliness. It’s usually considered when a client is committed to learning skills they can generalize to their life
outside therapydating, relationships, marriage, or simply being comfortable in their own skin.
How the triadic model actually works
“Three-person team” does not mean three people sitting in a room like an awkward group project. Typically, the therapist meets with the client separately
(talk therapy), and the surrogate partner meets with the client separately (experiential sessions). The therapist and surrogate communicate professionally
about goals and progress, within the boundaries the client agrees to.
The therapist’s role
- Assess whether SPT is appropriate (and screen out situations where it isn’t)
- Clarify goals: What exactly is changing? Comfort with touch? Ability to communicate needs? Reducing panic?
- Support integration: help the client process emotions, meaning-making, and relationship patterns
- Monitor ethics and safety: boundaries, consent, and clinical appropriateness
The surrogate partner’s role
- Provide structured experiential exercises aligned with the treatment plan
- Help the client practice communication, consent, boundaries, and intimacy skills
- Offer real-time feedback: “When you shut down, what do you notice in your body?”
- Move at the client’s pacestepwise, with explicit consent and check-ins
The client’s role
- Show up honestly (including about fear, shame, anger, attraction, confusionwhatever’s real)
- Practice skills inside sessions and apply them outside sessions
- Communicate boundaries and consent clearly (even when it’s uncomfortable)
- Do integration work with the therapist so experiences translate into lasting change
What happens in sessions?
Every ethical SPT process starts with a clear agreement: goals, boundaries, consent practices, privacy, health and safety expectations, and the “arc” of the work.
After that, sessions often follow a progressionlike learning to swim in the shallow end before anyone suggests a triathlon.
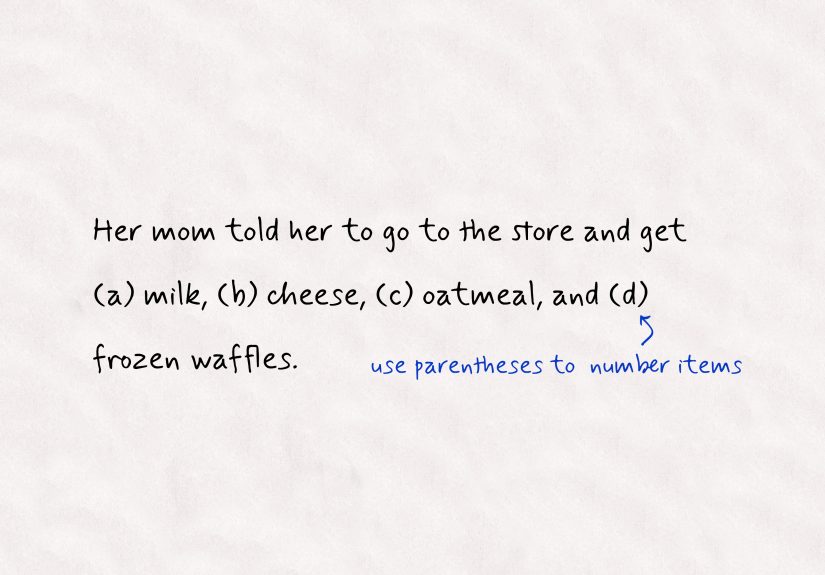
Examples of early-stage exercises
- Mindfulness and body awareness: noticing breath, tension, shutdown, or activation without judgment
- Communication drills: asking for what you want, saying “no,” negotiating “maybe,” practicing repair after discomfort
- Eye contact and presence: staying connected instead of dissociating or performing
- Boundary practice: “Stop,” “Slower,” “Different,” “That works,” “That doesn’t.”
Examples of mid-stage exercises
- Consensual touch practice: hand holding, hugging, non-sexual touch with clear permission and feedback
- Sensate-focus style exercises: exploring touch without performance pressure (often influenced by classic sex therapy methods)
- Body-image support: being seen in ways that feel safe and gradual, reducing shame
Later-stage work (when appropriate)
For some clients, the work may include sensual touch, arousal-focused exploration, or sexual contact. For others, “later-stage” might still be clothed touch,
comfortable nudity, or simply being able to stay present when intimacy increases.
The key point: the “finish line” is not the same for everyone. The finish line is the client’s goals, not a predetermined checklist.
Training, professionalism, and ethics
Surrogate partners are not universally regulated by a single U.S. licensing board the way psychologists or clinical social workers are. That makes
training and ethical structure especially important.
Some surrogate partners train through professional organizations that outline education, supervised practice, and ethics guidelines. Ethical frameworks emphasize
that the role “surrogate partner” applies within a supervised therapeutic triad and involves collaboration with a supervising therapist, not independent “sessions”
disconnected from care.
In reputable models, there are clear standards around consent, confidentiality, health and sexual safety practices, scope of practice, and planned termination of
the therapeutic relationship.
Is surrogate partner therapy legal in the U.S.?
This is where the answer gets annoyingbut honest: there isn’t one simple nationwide rule that covers every detail.
There is no single U.S. federal law that specifically defines “surrogate partner therapy” as legal or illegal. However, sexual services laws vary by state and
locality, and the line between therapeutic practice and illegal activity can be interpreted differently depending on context.
Some surrogate partner organizations argue that SPT itself is not illegal and emphasize its therapeutic structure. At the same time, legal and ethics scholars have
discussed the uncertainty and risk created by prostitution statutes, professional regulation differences, and the lack of standardized oversight.
If someone is considering SPT, it’s wise to consult a qualified clinician and, if needed, legal counsel familiar with local laws.
What does the research say? (Spoiler: more would be nice)
Research on SPT exists, but it’s not as robust as many people would like. Ethical complexity, privacy concerns, and the niche nature of the work make large,
randomized studies difficult.
That said, published clinical and scholarly discussions describe SPT as a structured intervention that can address barriers to intimacy through experiential learning,
and they highlight both potential benefits and real risks (boundary issues, emotional dependence, exploitation concerns, and legal ambiguity).
In other words: the concept aligns with what we know about exposure-based learning and skills practice, but the evidence base is still developingand quality care
depends heavily on ethics, training, and clinical judgment.
Benefits people often report
- Reduced anxiety around touch, nudity, or sexual performance
- Better communication and the ability to ask for needs without apologizing for existing
- Stronger boundary skills (saying no, renegotiating, speaking up early)
- Improved self-awareness of bodily cues (activation, shutdown, dissociation)
- More confidence dating or relating, because skills were practicednot just understood intellectually
Risks and concerns (the grown-up section)
Any therapy that involves intimacy deserves extra care. Potential risks include:
- Emotional attachment: feelings can deepen quickly; planned endings must be handled with support.
- Boundary confusion: without clear agreements, clients can feel pressuredor surrogates can be put in unsafe situations.
- Ethical drift: if a therapist isn’t trained in this modality, coordination can get messy fast.
- Power dynamics: the client is vulnerable; professionalism and consent practices matter immensely.
- Legal uncertainty: local laws differ, and risk tolerance varies.
The safest version of SPT is the boring-sounding one: a qualified therapist, clear documentation of goals, explicit consent practices, training verification,
and transparent boundaries. (Yes, “boring” can be a love language when safety is involved.)
How to find surrogate partner therapy the safer way
If you’re considering SPT, start with a licensed therapistideally a clinician with training in sex therapy. A reputable process usually includes:
- Assessment first: screening for trauma stability, coercion risk, active addiction concerns, or untreated mental health crises
- Clear goals: specific, measurable, and connected to daily life (not vague “be better at sex”)
- Verification of training: ask where and how the surrogate partner trained, and how supervision works
- Informed consent: explicit agreement about touch, pace, safer sex practices, confidentiality, and termination
- Ongoing integration: regular therapy sessions to process what comes up
Red flags include secrecy, pressure to “skip the therapist,” refusal to discuss consent practices, or anyone who guarantees a specific sexual outcome.
Therapy isn’t a vending machine: you don’t put in money and get out “confidence” in B6.
Frequently asked questions
Do surrogate partners always have sex with clients?
No. Some work includes sexual contact, but many cases focus on communication, touch tolerance, body image, or anxiety reduction without intercourse.
The scope depends on the treatment plan, client goals, and consent.
Is SPT only for single people?
It’s commonly framed for individuals, but circumstances vary. The defining feature is the triadic therapeutic structure and a clinician-guided plan, not a
relationship status label.
Is it covered by insurance?
Often, noespecially the surrogate partner component. Talk therapy may be covered depending on the clinician, diagnosis coding, and plan.
Clients should ask providers directly and plan for out-of-pocket costs.
What if I develop feelings?
That’s commonand it’s not “bad.” It’s information. A good therapist will help you understand what the feelings mean, how attachment patterns show up,
and how to translate growth into real relationships.
Bottom line
Surrogate Partner Therapy is a structured, clinician-guided way to practice intimacy skills in real timeespecially when talk therapy isn’t enough to shift
deeply embodied fear, shame, or avoidance. At its best, it’s careful, ethical, consent-based, and relentlessly focused on helping clients build capacity for
intimacy in their actual lives.
At its worst, if it’s done without proper training, boundaries, or clinical oversight, it can be confusing, risky, or exploitative. So if SPT is on your radar,
let “slow and qualified” be your filter.
Real-World Experiences: What it can feel like (500-word add-on)
Because SPT is private by nature, many people only “meet” it through headlines or film plotsneither of which are famous for nuance. So here are a few
composite, anonymized examples based on commonly described themes in clinical discussions and educational materials. These aren’t any one person’s story;
think of them like “patterns that show up,” not gossip.
Experience #1: “My body hits the panic button before my brain finishes the sentence.”
One client starts therapy saying, “I want intimacy, but the moment someone gets close, I freeze.” In talk therapy, they learn the historystrict rules about sex,
shame-based messages, a past relationship where consent wasn’t respected. They understand it intellectually. Their body does not care.
With a surrogate partner, the work begins almost comically small: sitting across from someone and practicing eye contact for 30 seconds. Naming sensations out loud:
“My chest is tight.” Learning to ask for a pause without apologizing. Over time, touch exercises are introduced with explicit consent and constant check-ins.
The client’s “panic button” still existsbut it becomes less sensitive. They learn what early activation feels like and how to regulate before they shut down.
Later, when they start dating, they recognize the signals sooner and communicate them clearly: “I’m into you, and I need to slow down.” That sentence alone
can be life-changing.
Experience #2: “I’ve never practiced this without feeling judged.”
Another client has a body that doesn’t match Hollywood’s idea of “sexy.” They’ve avoided dating for years because they assume rejection is guaranteed.
Talk therapy helps them challenge the story, but shame is stubborn.
Surrogate sessions focus on being seen gently and graduallystarting fully clothed, then practicing comfort with compliments, then consensual touch.
The surprising part isn’t the touch; it’s the feedback loop: the client learns that their needs can be heard without ridicule, and their body can be
engaged with respect rather than evaluation. They practice receiving pleasure without “earning it” through performance. Eventually, dating becomes less like an
audition and more like a conversation.
Experience #3: “I’m disabledand intimacy feels like a logistics nightmare.”
A client with a disability may want intimacy but feel anxious about the mechanics: positioning, fatigue, medical devices, fear of burdening a partner,
or worry that a new person will panic or pity them.
In a structured SPT approach, the client practices asking for accommodations and communicating needs clearly: “I need this angle,” “I need breaks,”
“Please don’t assume I’m fragileask.” That’s not just sexual skill; that’s relationship skill. The client leaves with scripts, confidence, and a stronger sense
of agencyplus the experience of being desired and respected in a way that’s often missing from everyday social spaces.
Experience #4: “The biggest win wasn’t sexit was boundaries.”
Many clients expect the breakthrough will be a sexual milestone. Sometimes it is. But often the deeper change is learning to say no, to renegotiate, to name
discomfort early, and to repair after missteps. That’s the stuff that makes long-term intimacy possible.
The common thread across experiences isn’t a specific actit’s capacity: the ability to stay present, communicate clearly, and feel safe enough in
your body to connect with another person without fear doing all the talking.