Table of Contents >> Show >> Hide
- Why diet matters for osteoporosis prevention
- The bone-building nutrients that actually move the needle
- What to eat for osteoporosis prevention
- What to avoid (or at least limit) for osteoporosis prevention
- How to build a bone-healthy plate (without turning meals into math)
- Special situations (because real life has plot twists)
- Experiences from real life (the “been there, crunched that” section)
- Experience #1: “I drink coffee all day, and somehow I’m still tired.”
- Experience #2: “I gave up dairy, so I guess I can’t get enough calcium.”
- Experience #3: “I eat ‘healthy’ but my sodium is sky-high.”
- Experience #4: “I take a handful of supplements, so I’m covered… right?”
- Experience #5: “I’m motivated… until dinner happens at 9 p.m.”
- Conclusion
Your skeleton is the only outfit you wear 24/7so it deserves better than a diet of iced coffee and “I’ll eat a vegetable later.”
Osteoporosis (literally “porous bones”) can sneak up quietly for years, then announce itself loudly with a fracture after a minor fall.
The good news: food choices really do matter for building and maintaining strong bonesespecially when you combine them with movement,
sleep, and a few strategic lifestyle swaps.
This guide breaks down what to eat more often, what to limit (not fear), and how to turn bone-health advice
into meals you’d actually want to repeat. Expect practical examples, label-reading tricks, and a tiny bit of humorbecause if we can’t laugh,
we’ll all cry into our calcium-fortified cereal.
Why diet matters for osteoporosis prevention
Bone isn’t a dead, dusty material like an old chalkboard. It’s living tissue that constantly remodelsold bone breaks down, new bone builds up.
Over time (and especially with aging, menopause, certain medications, low activity, or low nutrient intake), breakdown can outpace building.
Nutrition helps by supplying the raw materials and “helpers” your body needs to keep bone density as strong as possible.
Translation: osteoporosis prevention isn’t about one magic food. It’s about your overall patterndaily calcium sources, enough vitamin D to absorb
that calcium, adequate protein, plenty of produce, and fewer diet habits that quietly nudge your body toward bone loss.
The bone-building nutrients that actually move the needle
1) Calcium: the headline act
Calcium is the main mineral in your bones. If your diet doesn’t provide enough, your body can pull calcium from bone to keep blood levels stable.
Most adults need around 1,000 mg/day, while women over 50 and adults over 70 generally need about
1,200 mg/day. (Your exact target depends on age and sex.)
More is not always better. Very high intakesespecially from supplementscan cause problems for some people. Think “meet the goal,” not “win the Olympics.”
2) Vitamin D: calcium’s best friend
Vitamin D helps your body absorb calcium. Many adults do well aiming for about 600 IU (15 mcg) daily, and older adults often need
800 IU (20 mcg) daily. Food can help, but vitamin D is harder to “eat your way into” consistentlyso some people need fortified foods
and/or supplements, depending on their clinician’s guidance and labs.
3) Protein: not the villain
Bone has a protein framework (mostly collagen) that minerals attach to. Too little proteinespecially in older adultscan weaken muscles and raise fall risk.
Most people don’t need extreme “meat at every meal” plans, but they also shouldn’t be afraid of normal portions of protein from foods like dairy, eggs,
fish, beans, tofu, poultry, or lean meats.
4) The “supporting cast” nutrients
Bone health is a team sport. Helpful nutrients include:
- Vitamin K (leafy greens) to support bone proteins
- Magnesium (nuts, seeds, beans, whole grains) for bone structure and vitamin D metabolism
- Potassium (fruits and vegetables) often linked with healthier dietary patterns
- Phosphorus (common in many foods) which works with calciumusually not lacking in typical diets
What to eat for osteoporosis prevention
Calcium-rich foods you can build meals around
You don’t need a spreadsheet to get enough calciumbut you do need repeatable go-to foods. Here are options that make it easy:
Dairy (if you tolerate it)
- Milk (including lactose-free): about 300 mg calcium per cup
- Yogurt: often 250–400 mg per serving (check labels)
- Cheese: varies; hard cheeses are more concentrated
Fortified foods (the “helpful cheat code”)
- Fortified plant milks (soy, almond, oat): many provide calcium comparable to milk
- Fortified orange juice: useful if it fits your overall diet
- Fortified cereals: can contribute, but watch added sugar
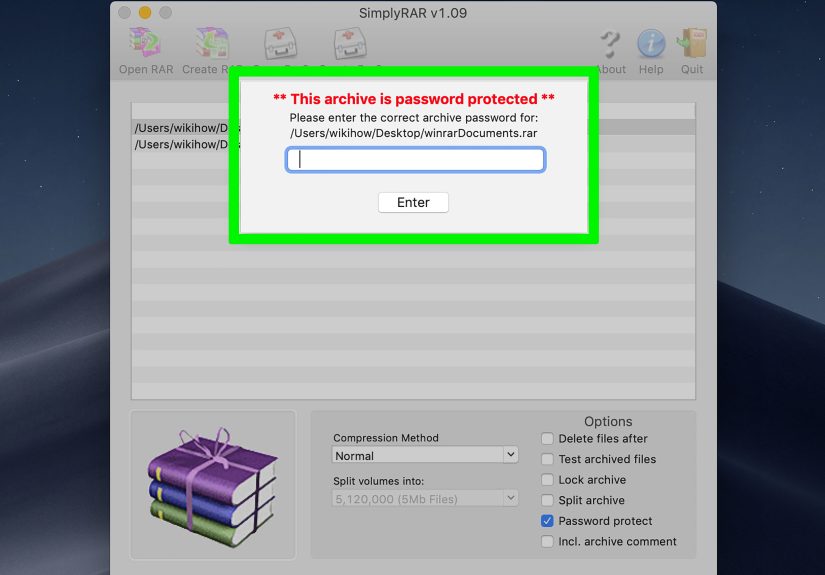
Label tip: look for calcium and vitamin D on the Nutrition Facts panel. Fortified products vary a lot by brand.
Fish with edible bones
- Canned salmon and sardines (bones included) can provide meaningful calcium
- Bonus: they also provide protein, and some types provide vitamin D
Plant-based calcium sources (yes, they count)
- Calcium-set tofu (made with calcium sulfate): often a strong source
- Beans and lentils: modest calcium plus magnesium and protein
- Chia and sesame/tahini: helpful boosts, especially in snacks
- Almonds: a “supporting” source (not usually enough alone)
Leafy greens: choose the right ones
Greens are fantasticjust know this: some have calcium that’s easier to absorb than others.
Spinach is high in calcium on paper, but it’s also high in oxalates, which bind calcium and reduce absorption.
Meanwhile, greens like kale, bok choy, and collards tend to be better “calcium deliverers.”
Vitamin D foods to put on repeat
- Fatty fish (like salmon)
- Egg yolks (modest amounts)
- Fortified milk and fortified plant milks
- Fortified cereals (again, choose lower-sugar options)
Fruits and vegetables: the underrated bone habit
Produce won’t replace calcium, but diets rich in fruits and vegetables are often linked with better overall nutrient intake (potassium, magnesium,
vitamin C) and healthier body composition and activity patterns. Plus, crunchy produce gives your jaw something to do besides clenching during
stressful emails.
What to avoid (or at least limit) for osteoporosis prevention
1) High-sodium diets
Sodium (salt) can increase calcium loss in urine. The bigger issue is where sodium comes from: processed foods, fast food, salty snacks, instant soups,
cured meats, and “it tasted bland so I panic-salted it.”
Bone-friendly move: emphasize whole foods and choose “low-sodium” versions when you can. Use flavor boosters like garlic, lemon, vinegar, pepper,
paprika, herbs, and parmesan (yes, a little cheese can be a strategic move).
2) Excess caffeine
Caffeine may slightly reduce calcium absorption, especially when calcium intake is low. You don’t have to break up with coffeejust don’t let
“cup number four” replace meals or crowd out calcium-rich foods. If you drink coffee or tea, consider pairing it with calcium (like milk or a fortified
alternative) and keep intake moderate.
3) Heavy alcohol intake
Heavy drinking is associated with bone loss and higher fall risk. If you drink, moderation mattersthink in the neighborhood of up to one drink
per day for women and up to two for men as a common guideline. If you don’t drink, you’re not missing a bone-health miracle.
4) “Calcium blockers” you don’t need to fearjust schedule smartly
Some foods contain compounds that can reduce calcium absorption when eaten at the same time:
- High-oxalate foods (like spinach) bind calcium
- High-phytate foods (like wheat bran) can also bind minerals
Reality check: these foods can still be part of a healthy diet. The practical approach is to avoid relying on them as your main calcium source and,
if needed, separate calcium supplements from high-bran meals.
5) Over-supplementing (a very American hobby)
Supplements can help when diet falls short, but mega-dosing can backfire. Calcium has an upper intake limit (which varies by age), and too much
supplemental calcium may increase constipation and, in some people, kidney stone risk. If you use calcium supplements, many clinicians suggest
splitting doses because absorption is best in smaller amounts (often around 500 mg at a time).
Bottom line: supplements should “fill gaps,” not replace food, and they should match your personal risk factors and medical guidance.
How to build a bone-healthy plate (without turning meals into math)
A simple daily blueprint
- 2–3 calcium moments per day (dairy or fortified alternative, tofu, canned fish with bones, or a calcium-forward snack)
- 1 vitamin D anchor (fatty fish or fortified foods; supplement if advised)
- Protein at each meal (doesn’t have to be hugejust consistent)
- Produce at most meals (especially colorful and leafy greens)
- Keep sodium, alcohol, and caffeine in the “reasonable” zone
One-day example menu
Breakfast: Greek yogurt parfait with berries, chia seeds, and a sprinkle of granola (choose lower-sugar). Coffee with milk or fortified soy milk.
Lunch: Kale-and-chickpea salad with olive oil/lemon dressing, pumpkin seeds, and a side of fortified plant milk or a small piece of cheese.
Snack: Calcium-set tofu “dip” (blended tofu + herbs + garlic) with veggies, or sardines on whole-grain toast if you’re adventurous.
Dinner: Salmon bowl: baked salmon, roasted broccoli, quinoa, and a tahini drizzle. Add fruit for dessert.
Special situations (because real life has plot twists)
If you’re lactose intolerant
- Try lactose-free milk or yogurt (often easier to tolerate)
- Use fortified plant milks with calcium + vitamin D
- Lean on calcium-set tofu and canned fish with bones
If you eat vegan or mostly plant-based
- Choose fortified beverages and foods intentionally (calcium + vitamin D)
- Prioritize low-oxalate greens (kale, bok choy, collards)
- Include protein sources daily (tofu, tempeh, beans, lentils)
If you take a blood thinner like warfarin
Don’t “avoid greens.” Instead, keep vitamin K intake consistent day to day and coordinate with your clinician, because vitamin K can
interact with certain anticoagulants.
Experiences from real life (the “been there, crunched that” section)
The internet loves simple rules“eat this, never eat that”but real people live in the messy middle. Below are common experiences dietitians and
clinicians hear from patients and clients, plus the practical moves that tend to work best. (These are composite scenarios, not medical advice for any
one person.)
Experience #1: “I drink coffee all day, and somehow I’m still tired.”
This person isn’t doomed by caffeine; they’re usually under-fueled. Coffee replaces breakfast, lunch is a vending-machine masterpiece, and calcium
intake ends up accidentally tiny. The bone-friendly fix is surprisingly unglamorous: add a real breakfast (yogurt, fortified smoothie, eggs + greens),
keep coffee to a moderate amount, and stop letting caffeine be a meal substitute. Many people also find that adding milk or a fortified alternative to
coffee is an easy “calcium moment” that doesn’t feel like a diet overhaul.
Experience #2: “I gave up dairy, so I guess I can’t get enough calcium.”
This is one of the most common myths. What usually helps is building a short, reliable list of non-dairy staples: fortified soy milk, calcium-set tofu,
chia or tahini in snacks, and leafy greens that actually deliver absorbable calcium (hello, bok choy). Once someone learns to read labelsspecifically
for calcium and vitamin Dcalcium intake becomes less mysterious and more like a routine. The emotional win is big: people stop feeling like they’re
failing at bone health and start feeling like they’re running a competent kitchen.
Experience #3: “I eat ‘healthy’ but my sodium is sky-high.”
Sodium sneaks in through sauces, soups, bread, deli meats, frozen meals, and restaurant food. People often think salt only counts if they add it with
their own handwhich is adorable, but incorrect. The fix isn’t bland sadness. It’s switching to low-sodium versions of favorites, using acid (lemon,
vinegar) and herbs for flavor, and picking a few default meals at home that are naturally lower in sodium. Many people report their taste buds adapt in
a couple of weeks, and suddenly restaurant food tastes like it was seasoned by a saltshaker with unresolved feelings.
Experience #4: “I take a handful of supplements, so I’m covered… right?”
Supplements feel reassuringlike a nutritional insurance policy. But the common real-life issue is doubling up: a multivitamin plus a calcium pill plus
a “bone health” product, all while also eating fortified foods. That can push total intake beyond what’s helpful. People do best when they treat
supplements as gap-fillers: calculate a rough estimate from food, then supplement only what’s missing, ideally with clinician input if osteoporosis risk
is high. Another practical tweak: splitting calcium doses (rather than taking a big one) can be gentler on the stomach and align with absorption limits.
Experience #5: “I’m motivated… until dinner happens at 9 p.m.”
Busy schedules are where nutrition plans go to die. What consistently works is making bone health automatic:
keep two calcium-rich staples always available (yogurt, fortified milk, tofu), buy one “lazy” produce option (pre-washed greens or frozen broccoli),
and choose one protein that cooks quickly (eggs, canned salmon, rotisserie chicken, beans). People who do this aren’t more disciplinedthey just
designed a kitchen that supports them when willpower is out of office.
The shared theme across these experiences is hopeful: osteoporosis prevention doesn’t require perfection. It requires repeatable basics
that survive real lifework stress, travel, tight budgets, and the occasional “I ate popcorn for dinner” moment.
Conclusion
If you want a bone-health strategy that’s actually doable, focus on the boring winners: meet your calcium needs most days, get enough vitamin D to
absorb it, include protein consistently, eat plenty of fruits and vegetables, and keep sodium, alcohol, and caffeine in a reasonable range.
You don’t need a “perfect” dietjust a pattern your bones can count on.